| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 靶点 |
Survivin (IC50 = 0.54 nM)
|
|---|---|
| 体外研究 (In Vitro) |
生存基因启动子驱动的荧光素酶报告基因活性不影响司潘溴铵 (YM155;30 μM)。通过对生存素基因启动子的转录抑制,sepantronium bromide 可显着降低 p53 缺陷的 PC-3 和 PPC-1 人 HRPC 细胞中内源性生存素的表达。 c-IAP2、XIAP、Bcl-2、Bcl-xL、Bad、α-肌动蛋白和 β-微管蛋白的蛋白表达不受 sepatrium bromide (100 nM) 的影响。 Sepatrium bromide 的 IC50 范围为 2.3 至 11 nM,可有效抑制人类癌细胞系(突变或截短的 p53),包括 PC-3、PPC-1、DU145、TSU-Pr1、22Rv1、SK-MEL-5 和 A375,分别。 1]。溴化隔膜 (YM155) 可增加 NSCLC 细胞的伽马射线敏感性。当分离溴化物和伽玛射线联合使用时,凋亡细胞的数量和 caspase-3 活性会增加。此外,溴化庚烷无法快速修复由辐射引起的核 DNA 双链断裂 [2]。
|
| 体内研究 (In Vivo) |
在 PC-3 异种移植物中,sepantronium bromide(YM155;3 和 10 mg/kg)可抑制肿瘤生长,而不会导致明显的体重减轻或血细胞计数降低。溴化蛇纹石广泛分散在人体的肿瘤组织中。在 PC-3 原位异种移植物中,溴化蛇在 5 mg/kg 剂量下显示出 80% TGI [1]。当与伽马射线结合时,spentronium bromide (YM155) 对裸鼠中的 H460 或 Calu6 异种移植物表现出强大的抗癌功效 [2]。在原位肾肿瘤和转移性肺肿瘤模型中,Sepantronium bromide (YM-155) 和 IL-2 进一步降低了肿瘤重量、肺转移和荧光素染色的肿瘤图片 [3]。
|
| 酶活实验 |
使用 Pyrobest 聚合酶和以下引物,通过 PCR 从人类基因组 DNA 中分离出 2,767 bp 的人类生存素基因启动子序列:5
γ-H2AX免疫荧光染色。[2] 细胞在两孔Lab Tec小室载玻片(Nunc)中生长至50%融合,然后在50 nmol/LYM155或载体存在下培养48小时,然后暴露于3 Gy的γ辐射。在此后的不同时间,它们在室温下用4%多聚甲醛固定10分钟,在4°C下用0.1%Triton X-100渗透10分钟,并在室温下暴露于5%脱脂奶粉中10分钟。用PBS洗涤载玻片,然后在室温下首先用1:300稀释的组蛋白γ-H2AX小鼠单克隆抗体孵育2小时,然后用1:700稀释的Alexa 488标记的小鼠IgG山羊抗体孵育1小时。将载玻片安装在荧光安装介质中,用配备LSM5 PASCAL系统的共聚焦激光扫描显微镜观察荧光信号。以×100的放大倍数检查了三个随机区域,每个区域包含=50个细胞。如前所述,将含有≥10个免疫反应灶的核计数为γ-H2AX阳性,并计算阳性细胞的百分比[2]。 |
| 细胞实验 |
将细胞以 5-40 × 103 的密度接种在 96 孔板中。将溶解有 YM155 的 DMSO 给予细胞 48 小时。然后,使用磺基罗丹明 B 测定法计算细胞计数。台盼蓝排斥染色用于测定细胞活力。[1]
在有或没有YM155的情况下培养48小时后,通过胰蛋白酶消化和离心(0.05%胰蛋白酶-EDTA)收集PC-3和PPC-1细胞,并将其重新悬浮在DMEM中。将细胞悬浮液用等体积的台盼蓝(0.4%工作溶液)稀释。在血细胞计数器上计数活细胞(未染色)和死细胞(染色),活细胞与细胞总数的比率表示为活细胞百分比。 半胱氨酸天冬氨酸蛋白酶-3活性的测量。[1] 根据制造商的说明,用CPP32/SCaspase-3荧光蛋白酶检测试剂盒(MBL)测量半胱氨酸天冬氨酸蛋白酶-3活性。在用YM155孵育48小时后,PC-3和PPC-1细胞在100μL细胞裂解缓冲液(随试剂盒提供)中裂解,得到等体积(50μL)的细胞裂解液(100μg蛋白质)。加入2倍反应缓冲液后,将混合物加入黑色96孔板中。然后以5 mL/孔的速度加入DEVD-AFC底物(附有试剂盒),并将混合物在37°C下孵育30分钟。用荧光分光光度计在390 nm的激发波长和460 nm的发射波长下对荧光发射进行定量。 体外细胞生长抑制试验。[1] YM155的抗增殖活性通过国家癌症研究所使用的方法进行测量。用YM155处理48小时后,通过磺基罗丹明B测定细胞计数。GI50值通过逻辑分析计算,即药物浓度导致对照细胞在药物孵育过程中净蛋白质增加(通过硫罗丹明B染色测量)减少50%。该测定一式三份,平均GI50值由四次独立测定的结果得出。 体外抗肿瘤活性的时间依赖性。[1] A549细胞用YM155、甲氨蝶呤或阿霉素处理。通过用新鲜培养基洗涤五次,在不同长度的暴露时间后去除每种化合物。在细胞处理开始后的72小时温育时,用Alamar Blue测定法(Serotec;参考文献22)测定所选化合物对细胞增殖的影响,每种浓度(n=1)两次。通过逻辑分析计算IC50。为了了解每种化合物的体外作用模式和药效学特性,以对数标度绘制了YM155、阿霉素(作为曲线下面积依赖性药物)和甲氨蝶呤(作为时间相关药物)的对数斜率(暴露时间)和对数斜率的倒数(A549抗增殖作用的IC50),并比较了三种药物的IC50暴露时间曲线的斜率。 |
| 动物实验 |
PC-3 s.c. (orthotopic) xenografts in male nude mice (BALB/c nu/nu)
5 mg/kg Subcutaneous injection as a 3-day continuous infusion per week for 3 weeks by an implanted micro-osmotic pump. For the in vivo experiments, YM155 was dissolved and diluted in saline immediately before administration. In vivo antitumor activities against PC-3 s.c. xenograft model.[1] Five-week-old male nude mice (BALB/c nu/nu) were used. PC-3 cells (2 × 106–3 × 106) were injected into the flanks of the mice and allowed to reach a tumor volume of >100 mm3 in tumor volume (length × width2 × 0.5). YM155 was s.c. administered as a 3-day continuous infusion per week for 2 weeks using an implanted micro-osmotic pump (Alzet model 1003D, Durect) or i.v. administered five times a week for 2 weeks. The percentage of tumor growth inhibition 14 days after initial YM155 administration was calculated for each group using the following formula: MTV = 100 × {1 − [(MTV of the treated group on day 14) − (MTV of the treated group on day 0)] / [(MTV of the control group on day 14) − (MTV of the control group on day 0)]}, where MTV is mean tumor volume. For both the frozen tumors and plasma samples, survivin expression levels were analyzed by Western blotting and YM155 drug concentration by high-performance liquid chromatography/triple quadrupole mass spectrometry (LC/MS/MS) using validated methods. In vivo antitumor activities against PC-3 orthotopic xenograft model. [1] For orthotopic implantation, a PC-3 cell suspension (1 × 106/20 μL per mouse) was injected into the prostate dorsolateral lobe (right side) of 7-week-old male nude mice (BALB/c nu/nu). Two weeks after implantation, YM155 was s.c. administered as a 3-day continuous infusion per week for 3 weeks at 5 mg/kg/d using an implanted micro-osmotic pump (Alzet model 1003D, Durect). Body weight was measured periodically starting from the first day of YM155 administration. Three weeks later, the tumors adhering to the prostate and seminal vesicle were taken and weighed as tumor weight. The antitumor activity of YM155 was expressed as a percentage of tumor growth inhibition calculated using the following formula: MTW = 100 × [1 − (MTW on day 21 of the treated group) / (MTW on day 21 of the control group)]. Evaluation of tumor growth in vivo. [2] Tumor cells (2 × 106) were injected s.c. into the right hind leg of 6-week-old female athymic nude mice (BALB/c nu/nu). Tumor volume was determined from caliper measurement of tumor length (L) and width (W) according to the formula LW2/2. Treatment was initiated when the tumors in each group of animals achieved an average volume of ∼200 to 250 mm3. Treatment groups (each containing eight mice) consisted of vehicle control (physiologic saline), YM155 alone, vehicle plus radiation, and YM155 plus radiation. Vehicle or YM155 at a dose of 5 mg/kg of body mass was administered over 7 consecutive days (days 1-7) with the use of an implanted micro-osmotic pump (Alzet model 1003D; Durect). Mice in the radiation groups received 10 Gy of γ-radiation from a cobalt irradiator either as a single fraction on day 3 of drug treatment or fractionated over 5 consecutive days (days 3 to 7); the radiation was targeted to the tumor, with the remainder of the body shielded with lead. Growth delay (GD) was calculated as the time required to achieve a 5-fold increase in volume for treated tumors minus that for control tumors. The enhancement factor was then determined as: (GDcombination − GDYM155)/GDradiation.[2] Luciferase-expressing RENCA cells were implanted to the subrenal capsule of the left kidney and tail vein, respectively, to produce a mouse RCC model with an orthotopic tumor and metastatic lung tumors. The mice were randomly divided into four groups with an even distribution of IVIS values. Group 1 received intraperitoneal (IP) injection of 100 μL of phosphate-buffered saline (PBS) as a vehicle control; group 2 received YM155 alone (1 mg/kg body weight per day for 1 week by IP injection); group 3 received IL-2 alone (6000 U of recombinant IL-2 by IP injection on days 0, 4, and 8 of treatment); and group 4, the combination therapy group, received YM155 and IL-2 (dose and dosing schedule the same as in group 2 plus group 3). Tumor imaging was performed and tumor volume was analyzed in all groups on day 14 post-treatment. The mice were sacrificed, and the weights of the orthotopic tumor in the left kidney and sections of bilateral lung tissues with metastatic growth were measured.[3] |
| 参考文献 |
|
| 其他信息 |
Sepantronium bromide is an organic bromide salt consisting of sepantronium cations and bromide anions. It has been found to selectively inhibit survivin (BIRC5) gene promoter activity and to down-regulate survivin in vitro, so leading to induction of apoptosis. It has a role as an antineoplastic agent, a survivin suppressant and an apoptosis inducer. It contains a sepantronium.
Sepantronium Bromide is a small-molecule proapoptotic agent with potential antineoplastic activity. Sepantronium bromide selectively inhibits survivin expression in tumor cells, resulting in inhibition of survivin antiapoptotic activity (via the extrinsic or intrinsic apoptotic pathways) and tumor cell apoptosis. Survivin, a member of the inhibitor of apoptosis (IAP) gene family, is expressed during embryonal development and is absent in most normal, terminally differentiated tissues; upregulated in a variety of human cancers, its expression in tumors is associated with a more aggressive phenotype, shorter survival times, and a decreased response to chemotherapy. Various accumulating evidence suggests that survivin, a member of the inhibitor of apoptosis (IAP) family, plays an important role in drug resistance and cancer cell survival in many types of cancer, including hormone-refractory prostate cancer (HRPC). Here, we characterized YM155, a novel small-molecule survivin suppressant, using a survivin gene promoter activity assay. YM155 suppressed expression of survivin and induced apoptosis in PC-3 and PPC-1 human HRPC cell lines at 10 nmol/L. In contrast, YM155 up to 100 nmol/L showed little effect on expression levels of other IAP- or Bcl-2-related proteins. In a s.c. xenografted PC-3 tumor model in mice, 3-day continuous infusions of YM155 at 3 to 10 mg/kg induced massive tumor regression accompanied by suppression of intratumoral survivin. YM155 also completely inhibited the growth of orthotopically xenografted PC-3 tumors. No significant decreases in body weight were observed in mice treated with YM155 during the experimental period. Pharmacokinetic analyses indicated that YM155 is highly distributed to tumors and at concentrations approximately 20-fold higher than those in plasma. Our findings represent the first attempt to show tumor regression and suppression of survivin in p53-deficient human HRPC cells by a single small molecular compound treatment. Further extensive investigation of YM155 in many types of cancer, including HRPC, seems to be worthwhile to develop this novel therapeutic approach.[1] Purpose: Survivin, a member of the inhibitor of apoptosis protein family, is an attractive target for cancer therapy. We have now investigated the effect of YM155, a small-molecule inhibitor of survivin expression, on the sensitivity of human non-small cell lung cancer (NSCLC) cell lines to gamma-radiation. Experimental design: The radiosensitizing effect of YM155 was evaluated on the basis of cell death, clonogenic survival, and progression of tumor xenografts. Radiation-induced DNA damage was evaluated on the basis of histone H2AX phosphorylation and foci formation. Results: YM155 induced down-regulation of survivin expression in NSCLC cells in a concentration- and time-dependent manner. A clonogenic survival assay revealed that YM155 increased the sensitivity of NSCLC cells to gamma-radiation in vitro. The combination of YM155 and gamma-radiation induced synergistic increases both in the number of apoptotic cells and in the activity of caspase-3. Immunofluorescence analysis of histone gamma-H2AX also showed that YM155 delayed the repair of radiation-induced double-strand breaks in nuclear DNA. Finally, combination therapy with YM155 and gamma-radiation delayed the growth of NSCLC tumor xenografts in nude mice to a greater extent than did either treatment modality alone. Conclusions: These results suggest that YM155 sensitizes NSCLC cells to radiation both in vitro and in vivo, and that this effect of YM155 is likely attributable, at least in part, to the inhibition of DNA repair and enhancement of apoptosis that result from the down-regulation of survivin expression. Combined treatment with YM155 and radiation warrants investigation in clinical trials as a potential anticancer strategy.[2] YM155, a small molecule inhibitor of the antiapoptotic protein survivin, has been developed as a potential anti-cancer drug. We investigated a combination therapy of YM155 and interleukin-2 (IL-2) in a mouse model of renal cell carcinoma (RCC). YM155 caused cell cycle arrest and apoptosis in renal cancer (RENCA) cells. Next, luciferase-expressing RENCA cells were implanted in the left kidney and the lung of BALB/c mice to develop RCC metastatic model. In this orthotopic renal and metastatic lung tumors models, YM155 and IL-2 additively decreased tumor weight, lung metastasis, and luciferin-stained tumor images. Also, the combination significantly suppressed regulatory T cells and myeloid-derived suppressor cells compared with single agent treatment. We suggest that a combination of YM155 and IL-2 can be tested as a potential therapeutic modality in patients with RCC.[3] |
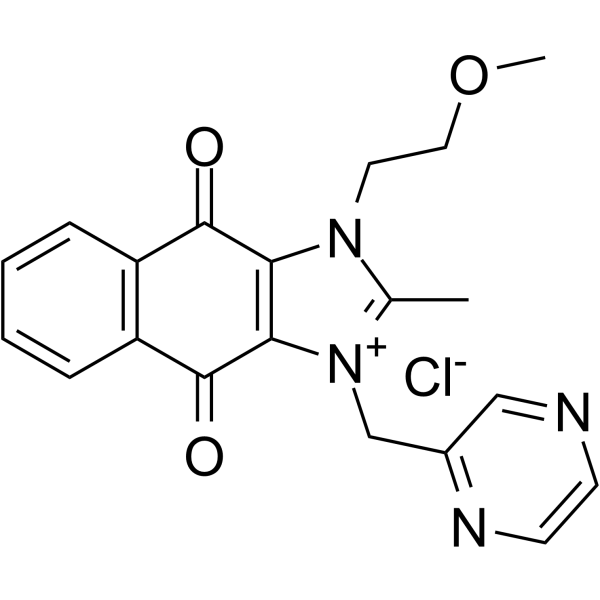
| 分子式 |
C20H19N4O3+.CL-
|
|---|---|
| 分子量 |
398.84286
|
| 精确质量 |
398.115
|
| 元素分析 |
C, 60.23; H, 4.80; Cl, 8.89; N, 14.05; O, 12.03
|
| CAS号 |
355406-09-6
|
| 相关CAS号 |
Sepantronium bromide;781661-94-7
|
| PubChem CID |
23108256
|
| 外观&性状 |
Light brown to brown solid powder
|
| tPSA |
77.96
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
28
|
| 分子复杂度/Complexity |
571
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
NUZWGSASIPTGSA-UHFFFAOYSA-M
|
| InChi Code |
InChI=1S/C20H19N4O3.ClH/c1-13-23(9-10-27-2)17-18(24(13)12-14-11-21-7-8-22-14)20(26)16-6-4-3-5-15(16)19(17)25;/h3-8,11H,9-10,12H2,1-2H3;1H/q+1;/p-1
|
| 化学名 |
1-(2-methoxyethyl)-2-methyl-3-(pyrazin-2-ylmethyl)benzo[f]benzimidazol-3-ium-4,9-dione;chloride
|
| 别名 |
YM-155 hydrochloride; 355406-09-6; YM-155 (hydrochloride); 1-(2-methoxyethyl)-2-methyl-4,9-dioxo-3-(pyrazin-2-ylmethyl)-4,9-dihydro-1H-naphtho[2,3-d]imidazol-3-ium chloride; Sepantronium (hydrochloride); 1-(2-methoxyethyl)-2-methyl-3-(pyrazin-2-ylmethyl)benzo[f]benzimidazol-3-ium-4,9-dione;chloride; YM-155hydrochloride; YM-155 (chloride);
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5073 mL | 12.5364 mL | 25.0727 mL | |
| 5 mM | 0.5015 mL | 2.5073 mL | 5.0145 mL | |
| 10 mM | 0.2507 mL | 1.2536 mL | 2.5073 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05263583 | Recruiting | Drug: Sepantronium Bromide | Burkitt Lymphoma Lymphoma, B-Cell |
Cothera Bioscience, Inc | December 9, 2022 | Phase 2 |
| NCT01023386 | Completed | Drug: YM155 | Cancer | Astellas Pharma Inc | November 2009 | Phase 1 |
| NCT01007292 | Completed | Drug: YM155 Biological: Rituximab |
Non-Hodgkin's Lymphoma | Novartis Pharmaceuticals | November 2009 | Phase 2 |
| NCT01009775 | Completed | Drug: YM155 Drug: Docetaxel |
Melanoma | Astellas Pharma Inc | November 2009 | Phase 2 |
| NCT01038804 | Completed | Drug: YM155 Drug: Docetaxel |
Breast Cancer | Astellas Pharma Inc | December 2009 | Phase 2 |