| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Sevoflurane is rapidly absorbed into circulation through the lungs; however, solubility in the blood is low (blood/gas partition coefficient at 37°C ranges from 0.63 to 0.69). Therefore, a minimal amount of sevoflurane needs to be dissolved in blood in order to induce anesthesia. The low solubility of sevoflurane facilitates its rapid elimination through the lungs, where 95% to 98% of this anesthetic is eliminated. Up to 3.5% of the sevoflurane dose appears in urine as inorganic fluoride, and as much as 50% of fluoride clearance is nonrenal (fluoride taken up into bone). Patients given low-flow sevoflurane anesthesia during maxillofacial surgery (n=16) had a peripheral volume of distribution of 1634 mlvapour/kgbw and a total volume of distribution of 1748 mlvapour/kgbw. In patients given low-flow sevoflurane anaesthesia during maxillofacial surgery (n=16), the transport clearance from the central to the peripheral compartment was 13.0 mlvapour/kgbw⋅min. Up to 3.5% of the sevoflurane dose appears in the urine as inorganic fluoride. Studies on fluoride indicate that up to 50% of fluoride clearance is nonrenal (via fluoride being taken up into bone). The low solubility of sevoflurane facilitates rapid elimination via the lungs. The rate of elimination is quantified as the rate of change of the alveolar (end-tidal) concentration following termination of anesthesia (FA), relative to the last alveolar concentration (FaO) measured immediately before discontinuance of the anesthetic. Fluoride ion concentrations are influenced by the duration of anesthesia, the concentration of sevoflurane administered, and the composition of the anesthetic gas mixture. In studies where anesthesia was maintained purely with sevoflurane for periods ranging from 1 to 6 hours, peak fluoride concentrations ranged between 12 uM and 90 uM. Peak concentrations occur within 2 hours of the end of anesthesia and are less than 25 uM (475 ng/mL) for the majority of the population after 10 hours. The concentrations of sevoflurane in milk are probably of no clinical importance 24 hours after anesthesia. Because of rapid washout, sevoflurane concentrations in milk are predicted to be below those found with many other volatile anesthetics. Compared with healthy individuals, the fluoride ion half-life was prolonged in patients with renal impairment, but not in the elderly. A study in 8 patients with hepatic impairment suggests a slight prolongation of the half-life. The mean half-life in patients with renal impairment averaged approximately 33 hours (range 21-61 hours) as compared to a mean of approximately 21 hours (range 10-48 hours) in normal healthy individuals. The mean half-life in the elderly (greater than 65 years) approximated 24 hours (range 18-72 hours). The mean half-life in individuals with hepatic impairment was 23 hours (range 16-47 hours). Metabolism / Metabolites Sevoflurane is metabolized to hexafluoroisopropanol by cytochrome P450 2E1 in a reaction that promotes the release of inorganic fluoride and carbon dioxide. Hexafluoroisopropanol is rapidly conjugated with glucuronic acid and eliminated in urine. _In vivo_ metabolism studies suggest that approximately 5% of the sevoflurane dose may be metabolized. In most cases, inorganic fluoride reaches its highest concentration within 2 hours of the end of sevoflurane anesthesia, and returns to baseline levels within 48 hours. Sevoflurane metabolism may be induced by chronic exposure to isoniazid and ethanol, and it has been shown that barbiturates do not affect it. Renal and hepatic toxicity of the fluorinated ether volatile anesthetics is caused by biotransformation to toxic metabolites. Metabolism also contributes significantly to the elimination pharmacokinetics of some volatile agents. Although innumerable studies have explored anesthetic metabolism in animals, there is little information on human volatile anesthetic metabolism with respect to comparative rates or the identity of the enzymes responsible for defluorination. The first purpose of this investigation was to compare the metabolism of the fluorinated ether anesthetics by human liver microsomes. The second purpose was to test the hypothesis that cytochrome P450 2E1 is the specific P450 isoform responsible for volatile anesthetic defluorination in humans. Microsomes were prepared from human livers. Anesthetic metabolism in microsomal incubations was measured by fluoride production. The strategy for evaluating the role of P450 2E1 in anesthetic defluorination involved three approaches: for a series of 12 human livers, correlation of microsomal defluorination rate with microsomal P450 2E1 content (measured by Western blot analysis), correlation of defluorination rate with microsomal P450 2E1 catalytic activity using marker substrates (para-nitrophenol hydroxylation and chlorzoxazone 6-hydroxylation), and chemical inhibition by P450 isoform-selective inhibitors. The rank order of anesthetic metabolism, assessed by fluoride production at saturating substrate concentrations, was methoxyflurane > sevoflurane > enflurane > isoflurane > desflurane > 0. There was a significant linear correlation of sevoflurane and methoxyflurane defluorination with antigenic P450 2E1 content (r = 0.98 and r = 0.72, respectively), but not with either P450 1A2 or P450 3A3/4. Comparison of anesthetic defluorination with either para-nitrophenol or chlorzoxazone hydroxylation showed a significant correlation for sevoflurane (r = 0.93, r = 0.95) and methoxyflurane (r = 0.78, r = 0.66). Sevoflurane defluorination was also highly correlated with that of enflurane (r = 0.93), which is known to be metabolized by human P450 2E1. Diethyldithiocarbamate, a selective inhibitor of P450 2E1, produced a concentration-dependent inhibition of sevoflurane, methoxyflurane, and isoflurane defluorination. No other isoform-selective inhibitor diminished the defluorination of sevoflurane, whereas methoxyflurane defluorination was inhibited by the selective P450 inhibitors furafylline (P450 1A2), sulfaphenazole (P450 2C9/10), and quinidine (P450 2D6) but to a much lesser extent than by diethyldithiocarbamate. These results demonstrate that cytochrome P450 2E1 is the principal, if not sole human liver microsomal enzyme catalyzing the defluorination of sevoflurane. P450 2E1 is the principal, but not exclusive enzyme responsible for the metabolism of methoxyflurane, which also appears to be catalyzed by P450s 1A2, 2C9/10, and 2D6. The data also suggest that P450 2E1 is responsible for a significant fraction of isoflurane metabolism. Identification of P450 2E1 as the major anesthetic metabolizing enzyme in humans provides a mechanistic understanding of clinical fluorinated ether anesthetic metabolism and toxicity. Sevoflurane, USP is metabolized to hexafluoroisopropanol (HFIP) with release of inorganic fluoride and CO2. Fluoride ion concentrations are influenced by the duration of anesthesia and the concentration of sevoflurane, USP. Once formed, HFIP is rapidly conjugated with glucuronic acid and eliminated as a urinary metabolite. No other metabolic pathways for sevoflurane, USP have been identified. In humans, the fluoride ion half-life was prolonged in patients with renal impairment, but human clinical trials contained no reports of toxicity associated with elevated fluoride ion levels. Cytochrome P450 2E1 is the principal isoform identified for sevoflurane metabolism and this may be induced by chronic exposure to isoniazid and ethanol. This is similar to the metabolism of isoflurane and enflurane and is distinct from that of methoxyflurane which is metabolized via a variety of cytochrome P450 isoforms. The metabolism of sevoflurane is not inducible by barbiturates. As shown in Figure 5, inorganic fluoride concentrations peak within 2 hours of the end of sevoflurane anesthesia and return to baseline concentrations within 48 hours post-anesthesia in the majority of cases (67%). The rapid and extensive pulmonary elimination of sevoflurane minimizes the amount of anesthetic available for metabolism. Sevoflurane is metabolized by cytochrome P450 2E1, to hexafluoroisopropanol (HFIP) with release of inorganic fluoride and CO2. Once formed HFIP is rapidly conjugated with glucuronic acid and eliminated as a urinary metabolite. No other metabolic pathways for sevoflurane have been identified. In vivo metabolism studies suggest that approximately 5% of the sevoflurane dose may be metabolized. In a study in which 4 dogs were exposed to 4% sevoflurane, USP for 3 hours, maximum serum fluoride concentrations of 17.0-27.0 umole/L were observed after 3 hours of anesthesia. Serum fluoride fell quickly after anesthesia ended, and had returned to baseline by 24 hours post-anesthesia. Relatively little biotransformation, only 5% is metabolized by cytochrome P450 CYP2E1 to hexafluoroisopropanol (HFIP) with release of inorganic fluoride and CO2. No other metabolic pathways have been identified for sevoflurane. Route of Elimination: The low solubility of sevoflurane facilitates rapid elimination via the lungs. In vivo metabolism studies suggest that approximately 5% of the sevoflurane dose may be metabolized. Up to 3.5% of the sevoflurane dose appears in the urine as inorganic fluoride. Half Life: 15-23 hours Biological Half-Life The terminal elimination half-life of sevoflurane from the peripheral fat compartment is approximately 20 hours. Compared with healthy individuals, the fluoride ion half-life was prolonged in patients with renal impairment, but not in the elderly. A study in 8 patients with hepatic impairment suggests a slight prolongation of the half-life. The mean half-life in patients with renal impairment averaged approximately 33 hours (range 21-61 hours) as compared to a mean of approximately 21 hours (range 10-48 hours) in normal healthy individuals. The mean half-life in the elderly (greater than 65 years) approximated 24 hours (range 18-72 hours). The mean half-life in individuals with hepatic impairment was 23 hours (range 16-47 hours). The half-life is in the range of 15-23 hours. |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Prospective, serial blood testing often demonstrates minor transient elevations in serum aminotransferase levels in the 1 to 2 weeks after major surgery. Appearance of ALT levels above 10 times the upper limit of normal, however, is distinctly unusual and points to significant hepatotoxicity. Clinically apparent, severe hepatic injury from sevoflurane is very rare, only isolated case reports having been published. The injury is marked by acute elevations in serum aminotransferase levels (5- to 50-fold) and appearance of jaundice within 2 to 21 days of surgery. There are usually minimal increases in alkaline phosphatase and gammaglutamyl transpeptidase levels. Jaundice is usually preceded by a day or two of fever and may be accompanied by rash and eosinophilia. The acute liver injury may be self-limited and resolve within 4 to 8 weeks, but can be severe and associated with acute liver failure. A strong risk factor is previous exposure to any of the halogenated anesthetics and particularly a history of halothane hepatitis or unexplained fever and rash after anesthesia with one of these agents. The differential diagnosis of acute liver injury after surgery and anesthesia is sometimes difficult, and a clinical picture similar to sevoflurane induced hepatitis can be caused by shock or ischemia, sepsis, other idiosyncratic forms of drug induced liver injury and acute viral or herpes hepatitis. Likelihood score: B (highly likely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation There is little published experience with sevoflurane during breastfeeding. Because the serum half-life of sevoflurane in the mother short and the drug is not expected to be absorbed by the infant, no waiting period or discarding of milk is required. Breastfeeding can be resumed as soon as the mother has recovered sufficiently from general anesthesia to nurse. When a combination of anesthetic agents is used for a procedure, follow the recommendations for the most problematic medication used during the procedure. General anesthesia for cesarean section using sevoflurane as a component may delay the onset of lactation. In one study, breastfeeding before general anesthesia induction reduced requirements of sevoflurane and propofol compared to those of nursing mothers whose breastfeeding was withheld or nonnursing women. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk A randomized study compared the effects of cesarean section using general anesthesia, spinal anesthesia, or epidural anesthesia, to normal vaginal delivery on serum prolactin and oxytocin as well as time to initiation of lactation. General anesthesia was performed using propofol 2 mg/kg and rocuronium 0.6 mg/kg for induction, followed by sevoflurane and rocuronium 0.15 mg/kg as needed. After delivery, patients in all groups received an infusion of oxytocin 30 international units in 1 L of saline, and 0.2 mg of methylergonovine if they were not hypertensive. Fentanyl 1 to 1.5 mcg/kg was administered after delivery to the general anesthesia group. Patients in the general anesthesia group (n = 21) had higher post-procedure prolactin levels and a longer mean time to lactation initiation (25 hours) than in the other groups (10.8 to 11.8 hours). Postpartum oxytocin levels in the nonmedicated vaginal delivery group were higher than in the general and spinal anesthesia groups. A retrospective study of women in a Turkish hospital who underwent elective cesarean section deliveries compared women who received bupivacaine spinal anesthesia (n = 170) to women who received general anesthesia (n = 78) with propofol for induction, sevoflurane for maintenance and fentanyl after delivery. No differences in breastfeeding rates were seen between the groups at 1 hour and 24 hours postpartum. However, at 6 months postpartum, 67% of women in the general anesthesia group were still breastfeeding compared to 81% in the spinal anesthesia group, which was a statistically significant difference. Protein Binding Sevoflurane protein binding has not been evaluated. _In vitro_ analyses have shown that other fluorinated volatile anesthetics can displace drugs from serum and tissue proteins; however, it is unclear if this is clinically significant. Clinical studies have shown that the administration of sevoflurane does not have a significant effect in patients taking drugs that are highly bound and have a small volume of distribution. |
| 其他信息 |
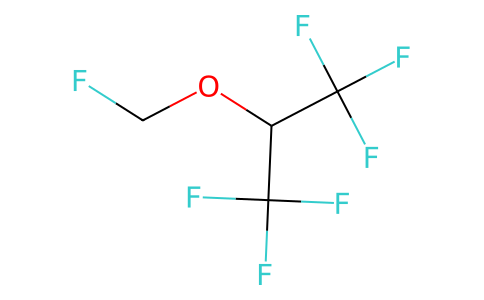
Sevoflurane is an ether compound having fluoromethyl and 1,1,1,3,3,3-hexafluoroisopropyl as the two alkyl groups. It has a role as an inhalation anaesthetic, a platelet aggregation inhibitor and a central nervous system depressant. It is an organofluorine compound and an ether. It is functionally related to a 2-methoxypropane.
Sevoflurane is an ether inhalation anesthetic agent used to induce and maintain general anesthesia. It is a volatile, non-flammable compound with a low solubility profile and blood/gas partition coefficient. Sevoflurane was patented in 1972, was approved for clinical use in Japan in 1990, and approved by the FDA in 1996. Sevoflurane is three times more potent than [desflurane], but has lower potency compared to [halothane] and [isoflurane]. Unlike other volatile anesthetics, sevoflurane has a pleasant odor and does not irritate the airway. The hemodynamic and respiratory depressive effects of sevoflurane are well tolerated, and most patients receiving this anesthetic agent present little toxicity. Therefore, it can be used for inhalational induction in adults and children for a wide variety of anesthetic procedures. Sevoflurane is a General Anesthetic. The physiologic effect of sevoflurane is by means of General Anesthesia. Sevofurane is one of the most commonly used volatile anesthetic agents, particularly for outpatient anesthesia and has an excellent safety record. Sevoflurane has been implicated in rare single case reports of severe acute liver injury similar to halothane hepatitis. Sevoflurane is a fluorinated isopropyl ether with general anesthetic property. Although the mechanism of action has not been fully elucidated, sevoflurane may act by interfering with the release and re-uptake of neurotransmitters at post-synaptic terminals, and/or alter ionic conductance following receptor activation by a neurotransmitter. Sevoflurane may also interact directly with lipid matrix of neuronal membranes, thereby affecting gating properties of ion channels. In addition, this agent may activate gamma-aminobutyric acid (GABA) receptors hyperpolarizing cell membranes. This results in a general anesthetic effect, a decrease in myocardial contractility and mean arterial pressure as well as an increased respiratory rate. Sevoflurane is only found in individuals that have used or taken this drug. Sevoflurane (2,2,2-trifluoro-1-[trifluoromethyl]ethyl fluoromethyl ether), also called fluoromethyl, is a sweet-smelling, non-flammable, highly fluorinated methyl isopropyl ether used for induction and maintenance of general anesthesia. Together with desflurane, it is replacing isoflurane and halothane in modern anesthesiology. [Wikipedia] Sevoflurane induces a reduction in junctional conductance by decreasing gap junction channel opening times and increasing gap junction channel closing times. Sevoflurane also activates calcium dependent ATPase in the sarcoplasmic reticulum by increasing the fluidity of the lipid membrane. It also appears to bind the D subunit of ATP synthase and NADH dehydogenase and also binds to the GABA receptor, the large conductance Ca2+ activated potassium channel, the glutamate receptor, and the glycine receptor. A non-explosive inhalation anesthetic used in the induction and maintenance of general anesthesia. It does not cause respiratory irritation and may also prevent PLATELET AGGREGATION. Drug Indication Sevoflurane is used for the induction and maintenance of general anesthesia in adult and pediatric patients for inpatient and outpatient surgery. For the induction and maintenance of anaesthesia. For the induction and maintenance of anaesthesia in dogs and cats. Mechanism of Action The precise mechanism of action of sevoflurane has not been fully elucidated. Like other halogenated inhalational anesthetics, sevoflurane induces anesthesia by binding to ligand-gated ion channels and blocking CNS neurotransmission. It has been suggested that inhaled anesthetics enhance inhibitory postsynaptic channel activity by binding GABAA and glycine receptors, and inhibit excitatory synaptic channel activity by binding nicotinic acetylcholine, serotonin, and glutamate receptors. Sevoflurane has an effect on several ionic currents, including the hyperpolarisation-activated cation current (If), the T-type and L-type Ca2+ currents (ICa, T and ICa, L), the slowly activating delayed rectifier K+ currents (IKs), and the Na+/Ca2+ exchange current (INCX). This ability to modulate ion channel activity can also regulate cardiac excitability and contractility. Sevoflurane is widely used as a volatile anesthetic in clinical practice. However, its mechanism is still unclear. ...It has been reported that voltage-gated sodium channels have important roles in anesthetic mechanisms. Much attention has been paid to the effects of sevoflurane on voltage-dependent sodium channels. To elucidate this, /investigators/ examined the effects of sevoflurane on Na(v) 1.8, Na(v) 1.4, and Na(v) 1.7 expressed in Xenopus oocytes. The effects of sevoflurane on Na(v) 1.8, Na(v) 1.4, and Na(v) 1.7 sodium channels were studied by an electrophysiology method using whole-cell, two-electrode voltage-clamp techniques in Xenopus oocytes. Sevoflurane at 1.0 mM inhibited the voltage-gated sodium channels Na(v)1.8, Na(v)1.4, and Na(v)1.7, but sevoflurane (0.5 mM) had little effect. This inhibitory effect of 1 mM sevoflurane was completely abolished by pretreatment with protein kinase C (PKC) inhibitor, bisindolylmaleimide I. Sevoflurane appears to have inhibitory effects on Na(v)1.8, Na(v)1.4, and Na(v) 1.7 by PKC pathways. However, these sodium channels might not be related to the clinical anesthetic effects of sevoflurane. Sevoflurane has been demonstrated to vasodilate the feto-placental vasculature. /Investigators/ aimed to determine the contribution of modulation of potassium and calcium channel function to the vasodilatory effect of sevoflurane in isolated human chorionic plate arterial rings. Quadruplicate ex vivo human chorionic plate arterial rings were used in all studies. Series 1 and 2 examined the role of the K+ channel in sevoflurane-mediated vasodilation. Separate experiments examined whether tetraethylammonium, which blocks large conductance calcium activated K+ (KCa++) channels (Series 1A+B) or glibenclamide, which blocks the ATP sensitive K+ (KATP) channel (Series 2), modulated sevoflurane-mediated vasodilation. Series 3 - 5 examined the role of the Ca++ channel in sevoflurane induced vasodilation. Separate experiments examined whether verapamil, which blocks the sarcolemmal voltage-operated Ca++ channel (Series 3), SK&F 96365 an inhibitor of sarcolemmal voltage-independent Ca++ channels (Series 4A+B), or ryanodine an inhibitor of the sarcoplasmic reticulum Ca++ channel (Series 5A+B), modulated sevoflurane-mediated vasodilation. Sevoflurane produced dose dependent vasodilatation of chorionic plate arterial rings in all studies. Prior blockade of the KCa++ and KATP channels augmented the vasodilator effects of sevoflurane. Furthermore, exposure of rings to sevoflurane in advance of TEA occluded the effects of TEA. Taken together, these findings suggest that sevoflurane blocks K+ channels. Blockade of the voltage-operated Ca++channels inhibited the vasodilator effects of sevoflurane. In contrast, blockade of the voltage-independent and sarcoplasmic reticulum Ca++channels did not alter sevoflurane vasodilation. Sevoflurane appears to block chorionic arterial KCa++ and KATP channels. Sevoflurane also blocks voltage-operated calcium channels, and exerts a net vasodilatory effect in the in vitro feto-placental circulation. Administration of sevoflurane at the onset of reperfusion has been confirmed to provide a cerebral protection. However, little is known about the mechanism. In this study, /investigators/ tested the hypothesis that sevoflurane postconditioning induces neuroprotection through the up-regulation hypoxia inducible factor-1 alpha (HIF-1 alpha) and heme oxygenase-1 (HO-1) involving phosphatidylinositol-3-kinase (PI3K)/Akt pathway. In the first experiment, male Sprague-Dawley rats were subjected to focal cerebral ischemia. Postconditioning was performed by exposure to 2.5% sevoflurane immediately at the onset of reperfusion. The mRNA and protein expression of HIF-1 alpha and its target gene, HO-1, intact neurons and the activity of caspase-3 was evaluated at 6, 24 and 72 hr after reperfusion. In the second experiment, ... the relationship between PI3K/Akt pathway and the expression of HIF-1alpha and HO-1 in the neuroprotection induced by sevoflurane /was investigated/. Cerebral infarct volume, apoptotic neuron and the expression of HIF-1alpha, HO-1 and p-Akt were evaluated at 24hr after reperfusion. Compared with the control group, sevoflurane postconditiong significantly ameliorated neuronal injury, up-regulated mRNA and protein levels of HIF-1 alpha and HO-1, inhibited the activity of caspase-3, and decreased the number of TUNEL-positive cells and infarct sizes. However, the selective PI3K inhibitor, wortmannin not only partly eliminated the neuroprotection of sevoflurane as shown by reducing infarct size and apoptotic neuronal cells, but also reversed the elevation of HIF-1 alpha, HO-1 and p-Akt expression in the ischemic penumbra induced by sevoflurane. Therefore, /the/ data demonstrates that the cerebral protection from sevoflurane postconditioning is partly mediated by PI3K/Akt pathway via the up-regulation of HIF-1 alpha and HO-1. Sevoflurane is widely used for anesthesia, and is commonly used together with opioids in clinical practice. However, the effects of sevoflurane on mu-opioid receptor (uOR) functions is still unclear. In this study, the effects of sevoflurane on uOR functions were analyzed by using Xenopus oocytes expressing a uOR fused to chimeric G alpha protein G(qi5) (uOR-G(qi5)). Sevoflurane by itself did not elicit any currents in oocytes expressing uOR-G(qi5), whereas sevoflurane inhibited the [D-Ala(2),N-Me-Phe(4),Gly(5)-ol]-enkephalin (DAMGO)-induced Cl(-) currents at clinically used concentrations. Sevoflurane did not affect the Cl(-) currents induced by AlF(4)(-), which directly led to activation of G proteins. The inhibitory effects of sevoflurane on the DAMGO-induced currents were not observed in oocytes pretreated with the protein kinase C (PKC) inhibitor GF109203X. These findings suggest that sevoflurane would inhibit uOR function. Further, the mechanism of inhibition by sevoflurane would be mediated by PKC. For more Mechanism of Action (Complete) data for Sevoflurane (9 total), please visit the HSDB record page. |
| 分子量 |
200.0548
|
|---|---|
| 精确质量 |
200.007
|
| CAS号 |
28523-86-6
|
| PubChem CID |
5206
|
| 外观&性状 |
Liquid
|
| 密度 |
1.4±0.1 g/cm3
|
| 沸点 |
49.5±35.0 °C at 760 mmHg
|
| 熔点 |
50-60ºC
|
| 闪点 |
-11.4±21.8 °C
|
| 蒸汽压 |
311.5±0.1 mmHg at 25°C
|
| 折射率 |
1.266
|
| LogP |
2.48
|
| tPSA |
9.23
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
8
|
| 可旋转键数目(RBC) |
2
|
| 重原子数目 |
12
|
| 分子复杂度/Complexity |
121
|
| 定义原子立体中心数目 |
0
|
| SMILES |
FC(C([H])(C(F)(F)F)OC([H])([H])F)(F)F
|
| InChi Key |
DFEYYRMXOJXZRJ-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C4H3F7O/c5-1-12-2(3(6,7)8)4(9,10)11/h2H,1H2
|
| 化学名 |
1,1,1,3,3,3-hexafluoro-2-(fluoromethoxy)propane
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 4.9988 mL | 24.9938 mL | 49.9875 mL | |
| 5 mM | 0.9998 mL | 4.9988 mL | 9.9975 mL | |
| 10 mM | 0.4999 mL | 2.4994 mL | 4.9988 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。