| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 靶点 |
HSP90α (IC50 = 7.8 nM); HSP90β (IC50 = 21 nM); GRP94 (IC50 = 535 nM); TRAP-1 (IC50 = 85 nM)
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
Luminespib 有效且选择性地抑制 HSP90,HSP90β 的 IC50 和 Ki 分别为 21 ± 16、8.2 ± 0.7 nM,HSP90α 的 IC50 和 Ki 为 7.8 ± 1.8、9.0 ± 5.0 nM。 Luminespib 对 GRP94 和 TRAP-1 具有弱活性,IC50 值分别为 535 ± 51 nM (Ki, 108 nM) 和 85 ± 8 nM (Ki, 53 nM)。 Luminespib 抑制各种人类肿瘤细胞系的增殖 (2.3–49.6 nM),诱导细胞周期停滞和细胞凋亡,并消耗人类癌细胞中的客户蛋白 (80 nM)[1]。 Luminespib (100 nM) 显着降低 CD40L 成纤维细胞诱导的免疫表型和 STAT3 信号传导变化,同时对 CLL 细胞的活力没有影响。 Luminespib (500 nM) 与 NSC 118218 联合使用比单独使用任一药物更有效地诱导共培养细胞凋亡,并且克服了成纤维细胞对 Hsp90 抑制剂的耐药性[2]。 Luminespib 对胰腺癌细胞具有很强的抑制作用,IC50 为 10 nM。无论存在或不存在 EGF,Luminespib (10 nM) 都能显着抑制胰腺癌细胞的迁移和侵袭 [3]。
|
||
| 体内研究 (In Vivo) |
在人类肿瘤异种移植物中,luminipespib(50、75 mg/kg,腹腔注射)有效抑制肿瘤生长速率,降低第 11 天的肿瘤平均重量[2]。在携带L3.6pl胰腺癌细胞的小鼠模型中,发光素(50 mg/kg/周,3×25 mg/kg/周)显着降低肿瘤重量和肿瘤生长速度[3]。
Luminespob/NVP-AUY922在体内对胰腺癌症细胞生长和血管形成的影响。为了评估NVP-AUY922在体内的生长抑制和抗血管生成作用,我们首先使用皮下肿瘤模型(L3.6pl细胞)。与对照组相比,NVP-AUY922(50mg/kg/周或3×25mg/kg/周)治疗显著降低了胰腺肿瘤的生长(图6A)。肿瘤生长的减少也反映在第17天切除肿瘤的最终重量上,NVP-AUY922治疗组的最终重量明显较低(图6B)。 为了测试Luminespib>/NVP-AUY922对HSP90的抑制是否确实在体内适当的肿瘤微环境中降低了胰腺癌症的生长,我们随后使用了胰腺癌症原位模型(L3.6pl细胞)。从肿瘤细胞植入后第7天开始,小鼠接受NVP-AUY922(50mg/kg)或赋形剂。在第26天,实验终止,因为对照组的小鼠因肿瘤负担而死亡。胰腺肿瘤负荷分析(肿瘤体积和肿瘤重量)表明,与对照组小鼠相比,Luminespib/NVP-AUY922治疗组小鼠的肿瘤明显较小(图6C和D)。重要的是,这两组小鼠的体重在统计学上没有差异。此外,在Luminespib/NVP-AUY922治疗组的肿瘤切片中,L3.6pl肿瘤的CD31阳性血管面积血管化显著减少。总之,这些结果表明,NVP-AUY922通过对肿瘤细胞的直接作用,以及通过抑制血管生成,显著抑制癌症的体内生长。3. 无胸腺小鼠每日服用Luminespib/NVP-AUY922(50mg/kg i.p.或i.v.),产生的峰值肿瘤水平至少比细胞GI高100倍(50)。这在具有不同致癌特征的人类肿瘤异种移植物中产生了统计学上显著的生长抑制和/或消退:BT474乳腺肿瘤治疗/对照组,21%;A2780卵巢,11%;U87MG胶质母细胞瘤7%;前列腺癌,37%;WM266.4黑色素瘤占31%。[1] NVP-AUY922抑制HSP90,并在人类肿瘤异种移植物中表现出强大的抗肿瘤功效。对携带BRAF突变体WM266.4黑色素瘤异种移植物的无胸腺小鼠进行5次每日腹腔注射50mg/kg NVP-AUY922后,液相色谱-串联质谱分析表明,24小时内肿瘤中NVP-AUYH22的浓度为6.8至7.7μmol/L(补充表S3)。通过电化学发光免疫测定定量,ERBB2水平在6小时时降至对照组的7.3%的最低点,在24小时内保持在35%以下。磷酸-ERK1/2水平为65%至83%,磷酸-AKT水平为13%至51%,AKT水平为57%至65%,HIF-1α水平为60%至85%。在24小时内,HSP72的表达增加到对照组的247%至281%。 [1] 测定了Luminespib/NVP-AUY922对已建立的WM266.4黑色素瘤异种移植物的治疗效果。每日剂量为75mg/kg,体重减轻约10%;因此,八次给药后剂量降至50mg/kg/d,体重迅速恢复。NVP-AUY922显著抑制了肿瘤生长速率,将对照组第11天的肿瘤平均重量从252±19mg降低到78±6mg(图5A)。第11天(最后一次给药后24小时)的肿瘤样本显示了耗竭ERBB2和CDK4的HSP90抑制特征,并诱导了HSP72(图5B)。[1] 研究人员接下来测试了每天腹腔注射或静脉注射50mg/kgLuminespib/NVP-AUY922对已建立的WM266.4黑色素瘤异种移植物的影响。治疗方案耐受良好,与对照组相比,平均体重无差异(i.p.)或差异<5%(i.v.)。与对照组相比,静脉注射组治疗9天后的肿瘤重量减轻了55%(P=0.000085),腹腔注射组减轻了46%(P=0.00067)。与之前的研究一样,生物标志物的变化证实了HSP90在肿瘤中的抑制作用。两种给药途径在肿瘤中产生了相当水平的NVP-AUY922(与上述单剂量研究中报告的水平相似),与观察到的相当疗效和药效学变化一致。在另外三项研究中,用不同的NVP-AUY922方案治疗患有WM266.4肿瘤的小鼠,在所有情况下,都观察到明显的生长延迟,在给药结束时生长率有所恢复(补充表S5)。 [1] 研究人员还测试了Luminespib/NVP-AUY922抑制已建立的播散性黑色素瘤的能力。静脉注射WM266.4黑色素瘤细胞后7天开始治疗,持续32天(50mg/kg,每周5次,持续18天,每周3次,再持续14天)。肺部组织学检查表明,NVP-AUY922治疗可减少肺转移的数量和大小(图5C)。如图5D所示,转移的平均数量从61±13减少到17±3(72%抑制;P=0.0037),转移所占的总面积从2.38±0.43 mm2减少到0.15±0.04 mm2(93.7%抑制;P=0.0003)。 [1] 然后,研究人员确定了Luminespib/NVP-AUY922在已建立的PTEN缺失U87MG人胶质母细胞瘤异种移植物中的疗效。再次获得高度显著的生长抑制;事实上,由于第18天的平均肿瘤体积降至第0天值的58%,因此观察到了回归(图6A)。Western blot证实HSP90抑制,ERBB2、AKT、磷酸化ERK1/2、HIF-1α和存活素显著减少,HSP72增加(数据未显示)。我们还发现组织切片中磷酸化AKT(Ser473)和磷酸化S6(Ser240/244)明显减少,这与磷脂酰肌醇3-激酶(PI3K)途径的抑制一致(图6B)。图6C显示,HIF-1α和AKT的水平分别降至对照组的39%和27%,HSP72的水平通过电化学发光免疫测定法增加了约800%。最后,NVP-AUY922治疗的肿瘤中微血管密度显著降低,表明具有抗血管生成作用(图6D)。 [1] 在U87MG异种移植物中进行了五天剂量(50mg/kg i.p.,与上述WM266.4相当)的平行药代动力学/药效学研究。最后一次给药后6至24小时,肿瘤Luminespib/NVP-AUY922的平均浓度为3.8至6.7μmol/L(补充表S4)。在6至24小时内,磷酸化AKT表达降至对照组的19%至56%,AKT降至74%至80%,HIF-1α降至32%至48%。该肿瘤中磷酸化ERK1/2水平明显没有降低,但HSP72表达增加至对照组的228%至530%(数据未显示)。 [1] 在不同组织起源和不同分子异常的其他人类肿瘤异种移植物中探索了Luminespib/NVP-AUY922的治疗效果。PTEN和PIK3CA突变型A2780卵巢癌[每天腹腔注射50mg/kg治疗8次后,治疗/对照(T/C)为10.5%;补充图S5A]和ERBB2+ERα+BT474乳腺癌(每天治疗24次后T/C为21%;补充图S52B)均显示出强烈的抑制作用。在后一种情况下,12个肿瘤中有5个出现了消退。体重减轻<5%,两项研究均获得了与HSP90抑制一致的明显生物标志物变化(补充图S5C和D)。在BT474中,除了CDK4和磷酸化ERK1/2的减少外,ERBB2完全丧失,ERα大量耗竭。 最后,研究人员在已建立的原位和转移性PTEN缺失的人前列腺癌异种移植物模型(PC3LN3)中探索了Luminespib/NVP-AUY922(每日腹腔注射50mg/kg)抑制生长和自发转移的能力。原发性肿瘤生长减少(补充图S6A),局部淋巴结转移的发生率和质量也降低(补充图S62B)。53%的对照组动物出现了远处淋巴结转移,但在NVP-AUY922治疗的动物中没有发现任何转移。Western印迹显示HSP72的诱导、ERBB2的强耗竭和CDK4的弱但可检测的耗竭(补充图S6C)。补充表S5总结了NVP-AUY922在所有测试的人类肿瘤异种移植物模型中的抗肿瘤活性。 |
||
| 酶活实验 |
对一组激酶进行了分析,并在Cerep对一组额外的酶和受体进行了筛选。X射线晶体学、荧光偏振和等温量热法如所述[1]。
|
||
| 细胞实验 |
分子生物标志物与肿瘤细胞和内皮细胞活性。[1]
测定了Luminespib/NVP-AUY922对人肿瘤和内皮细胞中客户端蛋白[如CRAF、BRAF、细胞周期蛋白依赖性激酶4(CDK4)、ERBB2、AKT和血管内皮生长因子受体2(VEGFR2)]表达和HSP72诱导的影响。肿瘤细胞趋化性、触敏性、侵袭性和与血管生成相关的内皮细胞功能也如所述进行了测定,但略有变化(见图图例)。 生物样本中Luminespib/NVP-AUY922的测量。[1] 用小鼠和人肝制剂进行微粒体培养,并如所述进行人癌细胞摄取研究。鉴于NVP-AUY922在HCT116结肠癌细胞中的GI50相对较低,我们使用5×GI50进行细胞摄取研究,并在HT29细胞中使用等摩尔浓度。[1] 3-(4,5-二甲基噻唑-2-基)-2,5-二苯基溴化四唑分析。[3] 为了评估Luminespib/NVP-AUY922的细胞毒性潜力,将胰腺癌症细胞以及HUVEC和VSMC接种到96细胞板(每孔1×103个细胞)中,并在37°C下暴露于不同浓度的NVP-AUY922指定时间。相应地向对照中加入相应浓度的DMSO。如前所述,使用3-(4,5-二甲基噻唑-2-基)-2,5-二苯基溴化四唑(MTT)测定法评估细胞存活率。 信号中间体的免疫印迹分析。[3] 为了确定Luminespib/NVP-AUY922对信号中间体的影响,进行了蛋白质印迹分析。实验进行了三次。除非另有说明,否则在用EGF(40ng/ml)、VEGF-A(50ng/ml)或PDGF-B(10ng/ml)刺激之前,将细胞与NVP-AUY922(10nmol/l)一起孵育20小时。全细胞裂解物和核提取物如别处所述制备。使用变性10%十二烷基硫酸钠聚丙烯酰胺凝胶对蛋白质样品(75μg)进行蛋白质印迹。依次用对磷酸化MEK、MEK、磷酸化AKTSer473、AKT、磷酸化ERKThr202/Tyr204、ERK、磷酸化信号转导子和转录激活子(STAT)3Tyr705、STAT3、HSP70、HER-2、cMET、粘着斑激酶(FAK)特异的抗体探测膜;磷酸化EGF-R2、VEGF-R2、磷酸化PDGF-Rβ、血小板源性生长因子-Rβ、β-肌动蛋白;HIF-1α)。通过增强化学发光检测抗体。如前所述,在组织裂解后,使用提取缓冲液对肿瘤组织样本进行蛋白质印迹分析。 运动性测定。[3] 为了确定Luminespib/NVP-AUY922(10 nmol/l)对体外细胞运动的影响,使用改良的Boyden室进行了迁移和侵袭试验,如别处所述。简而言之,将1×105个细胞重新悬浮在1%的FCS-DMEM中,并接种到具有8mm过孔的无涂层(迁移)或涂层(入侵)插入物中,以及10%的FCS-DME,含有或不含有EGF(40 ng/ml)、VEGF-A(50 ng/ml)或PDGF-B(10 ng/ml),作为化学引诱剂。24小时和48小时后,固定细胞并对迁移的细胞进行染色。在四个随机字段中计数细胞,并计算平均数量。 |
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
NVP-AUY922 shows limited metabolism and favorable pharmacokinetics. [1]
Incubation of 10 μmol/L NVP-AUY922 with mouse and human liver microsomes for 30 min resulted in 69 ± 4% and 59 ± 15% metabolism (mean ± SE, n = 3), respectively, considerably less than the isoxazole VER-50589, which showed 71 ± 5% metabolism at 5 min and complete metabolism after 15 min of incubation (34). The main NVP-AUY922 metabolites measured in mouse plasma were the glucuronide of the parent, a deethylated product, and an oxidation product. The glucuronide represented ∼95% of plasma metabolites as estimated by their area under the curves following i.v. and i.p. administration. Plasma pharmacokinetic variables compared well with those described for other pyrazole and isoxazole HSP90 inhibitors (31, 34), with similar fast clearances following both i.p. and i.v. administration to athymic mice bearing WM266.4 human melanomas (Fig. 4A–D). However, as predicted from its decreased metabolism and high cellular uptake, NVP-AUY922 showed enhanced tissue distribution with ratios of ≥4.0 in WM266.4 tumors, liver, and spleen compared with plasma following i.v. administration. Importantly, tumor clearance was significantly lower than that of normal tissues, with a longer terminal half-life of 14.7 to 15.5 h. This resulted in tumor NVP-AUY922 levels at least 100 × GI50 concentrations over 24 h following both i.v. and i.p. administration. Similar pharmacokinetic profiles were observed in other human tumor xenografts as indicated below. |
||
| 参考文献 |
|
||
| 其他信息 |
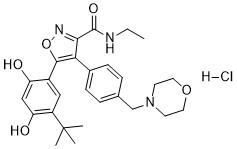
Luminespib is a monocarboxylic acid amide obtained by formal condensation of the carboxy group of 5-(2,4-dihydroxy-5-isopropylphenyl)-4-[4-(morpholin-4-ylmethyl)phenyl]-1,2-oxazole-3-carboxylic acid with the amino group of ethylamine. It has a role as a Hsp90 inhibitor, an antineoplastic agent and an angiogenesis inhibitor. It is a member of isoxazoles, a member of resorcinols, a member of morpholines, a monocarboxylic acid amide and an aromatic amide.
Luminespib is a derivative of 4,5-diarylisoxazole and a third-generation heat shock protein 90 (Hsp90) inhibitor with potential antineoplastic activity. Luminespib has been shown to bind with high affinity to and inhibit Hsp90, resulting in the proteasomal degradation of oncogenic client proteins; the inhibition of cell proliferation; and the elevation of heat shock protein 72 (Hsp72) in a wide range of human tumor cell lines. Hsp90, a 90 kDa molecular chaperone, plays a key role in the conformational maturation, stability and function of other substrate or "client" proteins within the cell, many of which are involved in signal transduction, cell cycle regulation and apoptosis, including kinases, transcription factors and hormone receptors. Hsp72 exhibits anti-apoptotic functions; its up-regulation may be used as a surrogate marker for Hsp90 inhibition. We describe the biological properties of NVP-AUY922, a novel resorcinylic isoxazole amide heat shock protein 90 (HSP90) inhibitor. NVP-AUY922 potently inhibits HSP90 (K(d) = 1.7 nmol/L) and proliferation of human tumor cells with GI(50) values of approximately 2 to 40 nmol/L, inducing G(1)-G(2) arrest and apoptosis. Activity is independent of NQO1/DT-diaphorase, maintained in drug-resistant cells and under hypoxic conditions. The molecular signature of HSP90 inhibition, comprising induced HSP72 and depleted client proteins, was readily demonstrable. NVP-AUY922 was glucuronidated less than previously described isoxazoles, yielding higher drug levels in human cancer cells and xenografts. Daily dosing of NVP-AUY922 (50 mg/kg i.p. or i.v.) to athymic mice generated peak tumor levels at least 100-fold above cellular GI(50). This produced statistically significant growth inhibition and/or regressions in human tumor xenografts with diverse oncogenic profiles: BT474 breast tumor treated/control, 21%; A2780 ovarian, 11%; U87MG glioblastoma, 7%; PC3 prostate, 37%; and WM266.4 melanoma, 31%. Therapeutic effects were concordant with changes in pharmacodynamic markers, including induction of HSP72 and depletion of ERBB2, CRAF, cyclin-dependent kinase 4, phospho-AKT/total AKT, and hypoxia-inducible factor-1alpha, determined by Western blot, electrochemiluminescent immunoassay, or immunohistochemistry. NVP-AUY922 also significantly inhibited tumor cell chemotaxis/invasion in vitro, WM266.4 melanoma lung metastases, and lymphatic metastases from orthotopically implanted PC3LN3 prostate carcinoma. NVP-AUY922 inhibited proliferation, chemomigration, and tubular differentiation of human endothelial cells and antiangiogenic activity was reflected in reduced microvessel density in tumor xenografts. Collectively, the data show that NVP-AUY922 is a potent, novel inhibitor of HSP90, acting via several processes (cytostasis, apoptosis, invasion, and angiogenesis) to inhibit tumor growth and metastasis. NVP-AUY922 has entered phase I clinical trials.[1] Chronic lymphocytic leukemia (CLL) involves disease infiltration into active proliferation centers within the lymph nodes and marrow. Successful treatment of CLL must involve targeting the leukemic cells in these supportive microenvironments. Our recent data suggest that inhibition of heat shock protein-90 (Hsp90) may be an effective treatment for CLL. We sought to further these data to determine whether the Hsp90 inhibitor, AUY922 (Novartis), is effective against CLL cells in a supportive in vitro environment. AUY922 significantly attenuated changes in immunophenotype and signal transducer and activator of transcription 3 (STAT3) signaling induced by CD40L-fibroblast co-culture but had no effect on the viability of CLL cells in this model. However, AUY922 in combination with fludarabine was significantly more effective at inducing apoptosis in cells in co-culture than either drug alone, an effect that was irrespective of ATM/TP53 dysfunction. In conclusion, our data suggest that further studies and clinical trials of AUY922 in combination with fludarabine may be warranted. [2] Aim: To evaluate the impact of heat-shock protein 90 (HSP90) blockade by the novel inhibitor NVP-AUY922, on tumor growth and angiogenesis in pancreatic cancer. Materials and methods: Effects of NVP-AUY922 on signaling pathways were evaluated by western blotting. Cell motility of cancer cells, pericytes and endothelial cells was investigated in Boyden chambers. Impact of HSP90 blockade on pancreatic tumor growth and angiogenesis were studied in in vivo tumor models. Results: NVP-AUY922 effectively inhibited cancer cell growth. Moreover, HSP90 inhibition potently interfered with multiple signaling pathways in cancer cells, as well as endothelial cells and pericytes, leading to significant reduction of pro-migratory and invasive properties of these cell types. In vivo, treatment with NVP-AUY922 significantly inhibited growth and vascularization of pancreatic cancer at doses far below the maximum tolerated dose. Conclusion: HSP90 blockade by the novel synthetic inhibitor NVP-AUY922 effectively reduces pancreatic cancer progression through direct effects on cancer cells, as well as on endothelial cells and pericytes.[3] |
| 分子式 |
C27H33N3O5
|
|---|---|
| 精确质量 |
479.242
|
| 元素分析 |
C, 62.84; H, 6.64; Cl, 6.87; N, 8.14; O, 15.50
|
| CAS号 |
747412-64-2
|
| 相关CAS号 |
747412-49-3; 1051919-21-1 (mesylate) ; 747412-64-2 (HCl); 1051919-26-6 (mesylate hydrate)
|
| PubChem CID |
135545855
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| LogP |
4.628
|
| tPSA |
108.06
|
| 氢键供体(HBD)数目 |
3
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
35
|
| 分子复杂度/Complexity |
687
|
| 定义原子立体中心数目 |
0
|
| SMILES |
CCNC(=O)C1=NOC(=C1C2=CC=C(C=C2)CN3CCOCC3)C4=CC(=C(C=C4O)O)C(C)(C)C
|
| InChi Key |
WLYWTGDTMWWNNG-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C27H33N3O5/c1-5-28-26(33)24-23(18-8-6-17(7-9-18)16-30-10-12-34-13-11-30)25(35-29-24)19-14-20(27(2,3)4)22(32)15-21(19)31/h6-9,14-15,31-32H,5,10-13,16H2,1-4H3,(H,28,33)
|
| 化学名 |
5-(5-tert-butyl-2,4-dihydroxyphenyl)-N-ethyl-4-[4-(morpholin-4-ylmethyl)phenyl]-1,2-oxazole-3-carboxamide
|
| 别名 |
747412-64-2; 5-(5-(tert-butyl)-2,4-dihydroxyphenyl)-N-ethyl-4-(4-(morpholinomethyl)phenyl)isoxazole-3-carboxamide; AUY 922; G1G66XE93W; 5-(5-tert-butyl-2,4-dihydroxyphenyl)-N-ethyl-4-[4-(morpholin-4-ylmethyl)phenyl]-1,2-oxazole-3-carboxamide; 3-Isoxazolecarboxamide, 5-(5-(1,1-dimethylethyl)-2,4-dihydroxyphenyl)-N-ethyl-4-(4-(4-morpholinylmethyl)phenyl)-; UNII-G1G66XE93W; Isoxazole, 40g;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。