| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|
| 靶点 |
HIV-1
MMP-2 |
|---|---|
| 体外研究 (In Vitro) |
Indinavir(0-50 µM;18 小时)抑制 PBMC 中淋巴细胞周期的 G0/G1 期,并降低细胞增殖能力 [1]。
Huh7 和 SK-HEP-1 肝癌细胞的细胞体外茚地那韦(40 µM–40 nM;5 天)和 40 µM–40 nM(48 小时)分别抑制侵袭和 MMPs-2 激活[2]。 |
| 体内研究 (In Vivo) |
Indinavir(70 mg/kg;ig;每天一次,持续 3 周)可抑制体内肝癌细胞的生长[2]。
|
| 细胞实验 |
细胞系:PBMC(来自健康和感染 HIV 的志愿者)
浓度:0-50 µM 孵育时间:18 小时(预处理;用抗 CD3 刺激另外 48 小时) 结果:封闭抗CD3以剂量依赖性方式诱导细胞周期进程。导致淋巴细胞增殖反应的剂量依赖性减少。 |
| 动物实验 |
Animal Model: Nude mice(s.c. into Huh7 and SK-HEP-1 cells)[2].
Dosage: 70 mg/kg Administration: Oral gavage; once a day for 3 weeks. Result: Compared to placebo, delayed the growth of s.c. implanted hepatocarcinoma xenografts in naked mice. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Rapidly absorbed Less than 20% of indinavir is excreted unchanged in the urine. Metabolism / Metabolites Hepatic. Seven metabolites have been identified, one glucuronide conjugate and six oxidative metabolites. In vitro studies indicate that cytochrome P-450 3A4 (CYP3A4) is the major enzyme responsible for formation of the oxidative metabolites. Indinavir has known human metabolites that include 1-[4-benzyl-2-hydroxy-5-[(2-hydroxy-2,3-dihydro-1H-inden-1-yl)amino]-5-oxopentyl]-N-tert-butyl-4-[(1-oxidopyridin-1-ium-3-yl)methyl]piperazine-2-carboxamide, N-tert-butyl-1-[2-hydroxy-5-[(2-hydroxy-2,3-dihydro-1H-inden-1-yl)amino]-4-[(4-hydroxyphenyl)methyl]-5-oxopentyl]-4-(pyridin-3-ylmethyl)piperazine-2-carboxamide, 1-[4-Benzyl-2-hydroxy-5-[(2-hydroxy-2,3-dihydro-1H-inden-1-yl)amino]-5-oxopentyl]-N-tert-butylpiperazine-2-carboxamide, and 1-[4-benzyl-5-[(2,3-dihydroxy-2,3-dihydro-1H-inden-1-yl)amino]-2-hydroxy-5-oxopentyl]-N-tert-butyl-4-(pyridin-3-ylmethyl)piperazine-2-carboxamide. Biological Half-Life 1.8 (± 0.4) hours |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Some degree of serum aminotransferase elevations occur in a high proportion of patients taking indinavir containing antiretroviral regimens. Moderate-to severe elevations in serum aminotransferase levels (>5 times the upper limit of normal) are found in 3% to 10% of patients, although rates may be higher in patients with HIV-HCV coinfection. These elevations are usually asymptomatic and self-limited and can resolve even with continuation of the medication. Indinavir therapy also causes increases in unconjugated (indirect) and total serum bilirubin that can manifest as jaundice in up to 10% of patients. These elevations are due to the inhibition of UDP glucuronyl transferase, the hepatic enzyme responsible for conjugation of bilirubin that is deficient in Gilbert syndrome. The hyperbilirubinemia is usually mild, the increases averaging 0.3-0.5 mg/dL, but can be more marked in patients with Gilbert syndrome with increases of 1.5 mg/dL or more and clinical jaundice. The jaundice, however, is not indicative of hepatic injury. Clinically apparent acute liver injury due to indinavir is rare. The few cases that have been reported have arisen after 1 to 8 weeks of starting indinavir, and the pattern of serum enzyme elevations has varied from hepatocellular to cholestatic. Signs of hypersensitivity (fever, rash, eosinophilia) are rare as is autoantibody formation. The acute liver injury due to indinavir is usually self-limited, but it can be severe, and isolated cases of acute liver failure have been reported. In addition, initiation of indinavir based highly active antiretroviral therapy can lead to exacerbation of an underlying chronic hepatitis B or C in coinfected individuals, typically arising 2 to 12 months after starting therapy and associated with a hepatocellular pattern of serum enzyme elevations and increases in serum levels of hepatitis B virus (HBV) DNA or hepatitis C virus (HCV) RNA. Indinavir therapy has not been clearly linked to lactic acidosis and acute fatty liver that is reported in association with several nucleoside analogue reverse transcriptase inhibitors. Likelihood score: C (frequent cause of serum bilirubin elevations and probable cause of rare instances of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Indinavir is no longer marketed in the US. Published experience with indinavir during breastfeeding is limited, but some infants may achieve high levels of the drug in breastmilk. Indinavir is not a recommended agent during breastfeeding. Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Gynecomastia has been reported among men receiving highly active antiretroviral therapy. Gynecomastia is unilateral initially, but progresses to bilateral in about half of cases. No alterations in serum prolactin were noted and spontaneous resolution usually occurred within one year, even with continuation of the regimen. Some case reports and in vitro studies have suggested that protease inhibitors might cause hyperprolactinemia and galactorrhea in some male patients, although this has been disputed. The relevance of these findings to nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. Protein Binding 60% |
| 参考文献 |
|
| 其他信息 |
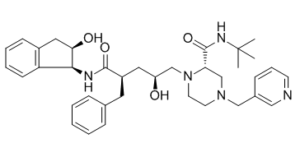
Indinavir is a N-(2-hydroxyethyl)piperazine, a piperazinecarboxamide and a dicarboxylic acid diamide. It has a role as a HIV protease inhibitor.
Indinavir anhydrous is a Protease Inhibitor. The mechanism of action of indinavir anhydrous is as a HIV Protease Inhibitor, and Cytochrome P450 3A4 Inhibitor. Indinavir is an antiretroviral protease inhibitor used in the therapy and prevention of human immunodeficiency virus (HIV) infection and the acquired immunodeficiency syndrome (AIDS). Indinavir can cause transient and usually asymptomatic elevations in serum aminotransferase levels and mild elevations in indirect bilirubin concentration. Indinavir is a rare cause of clinically apparent, acute liver injury. In HBV or HCV coinfected patients, antiretroviral therapy with indinavir may result in an exacerbation of the underlying chronic hepatitis B or C. Indinavir has been reported in Streptomyces with data available. Indinavir is a synthetic hydroxyaminopentane amide agent that selectively inhibits the protease of both human immunodeficiency virus 1 and 2. The incorporation of a basic amine into the hydroxyethylene backbone improves its aqueous solubility and its oral bioavailability. Indinavir Anhydrous is an anhydrous formulation of indinavir, a synthetic hydroxyaminopentane amide agent that selectively inhibits the protease of both human immunodeficiency virus 1 and 2. The incorporation of a basic amine into the hydroxyethylene backbone improves its aqueous solubility and its oral bioavailability. A potent and specific HIV protease inhibitor that appears to have good oral bioavailability. Drug Indication Indinavir is an antiretroviral drug for the treatment of HIV infection. FDA Label Crixivan is indicated in combination with antiretroviral nucleoside analogues for the treatment of HIV-1 infected adults. , Mechanism of Action Indinavir inhibits the HIV viral protease enzyme which prevents cleavage of the gag-pol polyprotein, resulting in noninfectious, immature viral particles. Pharmacodynamics Indinavir is a protease inhibitor with activity against Human Immunodeficiency Virus Type 1 (HIV-1). Protease inhibitors block the part of HIV called protease. HIV-1 protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious HIV-1. Indinavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles. Protease inhibitors are almost always used in combination with at least two other anti-HIV drugs. |
| 分子式 |
C36H47N5O4
|
|---|---|
| 分子量 |
613.79
|
| 精确质量 |
613.362
|
| 元素分析 |
C, 70.45; H, 7.72; N, 11.41; O, 10.43
|
| CAS号 |
150378-17-9
|
| 相关CAS号 |
Indinavir sulfate;157810-81-6;Indinavir sulfate ethanolate;2563866-80-6;Indinavir-d6;185897-02-3
|
| PubChem CID |
5362440
|
| 外观&性状 |
Solid powder
|
| 密度 |
1.2±0.1 g/cm3
|
| 沸点 |
831.6±75.0 °C at 760 mmHg
|
| 熔点 |
150-153ºC
|
| 闪点 |
456.8±37.1 °C
|
| 蒸汽压 |
0.0±3.2 mmHg at 25°C
|
| 折射率 |
1.629
|
| LogP |
4.04
|
| tPSA |
118.03
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
12
|
| 重原子数目 |
45
|
| 分子复杂度/Complexity |
952
|
| 定义原子立体中心数目 |
5
|
| SMILES |
O=C([C@@H](C[C@H](O)CN(CCN(CC1=CN=CC=C1)C2)[C@@H]2C(NC(C)(C)C)=O)CC3=CC=CC=C3)N[C@H]4C(C=CC=C5)=C5C[C@H]4O
|
| InChi Key |
CBVCZFGXHXORBI-PXQQMZJSSA-N
|
| InChi Code |
InChI=1S/C36H47N5O4/c1-36(2,3)39-35(45)31-24-40(22-26-12-9-15-37-21-26)16-17-41(31)23-29(42)19-28(18-25-10-5-4-6-11-25)34(44)38-33-30-14-8-7-13-27(30)20-32(33)43/h4-15,21,28-29,31-33,42-43H,16-20,22-24H2,1-3H3,(H,38,44)(H,39,45)/t28-,29+,31+,32-,33+/m1/s1
|
| 化学名 |
(2S)-1-[(2S,4R)-4-benzyl-2-hydroxy-5-[[(1S,2R)-2-hydroxy-2,3-dihydro-1H-inden-1-yl]amino]-5-oxopentyl]-N-tert-butyl-4-(pyridin-3-ylmethyl)piperazine-2-carboxamide
|
| 别名 |
trade name: Crixivan; DRG-0233; L-735 524; DRG0233; MK-639; L 735 524; MK 639; DRG 233; L735 524; MK639;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.6292 mL | 8.1461 mL | 16.2922 mL | |
| 5 mM | 0.3258 mL | 1.6292 mL | 3.2584 mL | |
| 10 mM | 0.1629 mL | 0.8146 mL | 1.6292 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Protease-inhibitor interactions.J Mol Biol.2005 Dec 9;354(4):789-800. |
The catalytic site of PRL24I–p2/NC at 1.1 Å resolution.J Mol Biol.2005 Dec 9;354(4):789-800. |
Structural differences at sites of mutation.J Mol Biol.2005 Dec 9;354(4):789-800. |