| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5g |
|
||
| 10g |
|

| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Topically, chlorhexidine is unlikely to undergo any degree of systemic absorption. Orally administered chlorhexidine, such as that found in oral rinses for dental purposes, is very poorly absorbed from the gastrointestinal tract - the Cmax in human subjects following an oral dose of 300mg was 0.206 µg/g and occurred approximately 30 minutes after ingestion (Tmax). Following the insertion of 4 PerioChips in 18 adult patients, no detectable plasma or urine chlorhexidine levels were observed. Excretion of chlorhexidine gluconate occurs almost exclusively via the feces, with less than 1% of an ingested dose excreted in the urine. 34 newborn infants who had been bathed in a standard manner with Hibiscrub were studied to find out whether it was absorbed percutaneously. Low levels of chlorhexidine were found in the blood of all 10 babies sampled by heel prick, and 5 of 24 from whom venous blood was taken. /Chlorhexidine gluconate/ Percutaneous absorption of the antimicrobial agent chlorhexidine (labelled with carbon-14) was studied in rats. Less than 5% of the topically applied chlorhexidine was absorbed during a 5-day period. Excretion of absorbed radioactivity occurred mainly in the feces. The percutaneous absorption of chlorhexidine gluconate (chlorhexidine digluconate; Hibitane) through hairless rat skin with or without stratum corneum was studied. For tests carried out on whole skin, storage in cutaneous structures after 48 hr was more important than diffusion; the reverse was observed for stripped skin. When the skin was stripped, the amount absorbed was multiplied by approximately 100, and the amount stored in skin by approximately 10. The difference in chlorhexidine diffusion observed between whole and stripped skin was related to the physicochemical characteristics of chlorhexidine. /Chlorhexidine gluconate/ To evaluate the elimination kinetics of chlorhexidine in milk when used as an intramammary infusion to stop lactation in cows. ... The study was performed in 2 phases. Three cows were studied in each phase. All cows were treated with chlorhexidine suspension by infusion into a mastitic mammary gland quarter after 2 milkings 24 hours apart. Foremilk samples (100 mL) were collected from treated and untreated (controls) mammary gland quarters of each cow. Chlorhexidine was extracted from raw milk, and residue concentrations were quantified by use of high-performance liquid chromatography. Foremilk samples from days 2, 5, and 8 were analyzed in phase I, and samples from time 0 and days 3, 7, 14, 21, 28, 35, and 42 were analyzed in phase II. In phases I and II, there was no quantifiable transference of chlorhexidine to milk in untreated mammary gland quarters. Measurable chlorhexidine residues were found in milk from treated mammary gland quarters of 2 cows throughout the 42-day sample period in phase II. Estimated mean elimination half-life for chlorhexidine in milk was 11.5 days. Metabolism / Metabolites As chlorhexidine is very poorly absorbed in the gastrointestinal tract, it is unlikely to undergo metabolic conversion to any significant extent. Biological Half-Life To evaluate the elimination kinetics of chlorhexidine in milk when used as an intramammary infusion to stop lactation in cows. ... The study was performed in 2 phases. Three cows were studied in each phase. All cows were treated with chlorhexidine suspension by infusion into a mastitic mammary gland quarter after 2 milkings 24 hours apart. Foremilk samples (100 mL) were collected from treated and untreated (controls) mammary gland quarters of each cow. Chlorhexidine was extracted from raw milk, and residue concentrations were quantified by use of high-performance liquid chromatography. Foremilk samples from days 2, 5, and 8 were analyzed in phase I, and samples from time 0 and days 3, 7, 14, 21, 28, 35, and 42 were analyzed in phase II. In phases I and II, there was no quantifiable transference of chlorhexidine to milk in untreated mammary gland quarters. Measurable chlorhexidine residues were found in milk from treated mammary gland quarters of 2 cows throughout the 42-day sample period in phase II. Estimated mean elimination half-life for chlorhexidine in milk was 11.5 days. |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Chlorhexidine has been used vaginally or topically on the abdomen or perineum prior to delivery to prevent infection. No toxicity has been reported in breastfed infants and it has clearly less toxicity compared to povidone-iodine in these situations. Topical application of chlorhexidine to the breast before and after nursing did not appear to adversely affect the breastfed infants in one study. Use of chlorhexidine oral rinse by a nursing mother is unlikely to adversely affect her infant. ◉ Effects in Breastfed Infants A group of investigators in Belgium reviewed the results of infant thyrotropin levels on day 5 postpartum in 4745 newborn infants delivered over a 2-year period at their hospital. Infants were divided among those whose mothers had iodine overload (n = 3086) from topical povidone-iodine 10% solution during labor and delivery and those whose mothers had no iodine overload (n = 1659). Mothers had povidone-iodine applied either as a single application to 900 square cm for epidural anesthesia or 3 applications to the entire abdominal wall for cesarean section. Breastfed infants whose mothers had iodine overload had a greater risk for having elevated thyrotropin levels and requiring recall for retesting (3.2% with cesarean section and 2.7% with epidural anesthesia) compared to those who did not (0.1%). Bottle-fed infants were affected much less than breastfed infants. After replacing povidone-iodine with chlorhexidine 0.5% in 70% isopropanol for disinfection for 6 months, 1178 infants that were delivered at this institution had no increased rate of elevations in thyroid function tests and a reduced rate of recalls in breastfed infants. In a study of mothers in Spain who received 10% povidone-iodine (n = 21) or chlorhexidine (n = 13) topically to the perineum starting immediately before the final stage of labor and daily postpartum to the episiotomy, no differences in thyrotropin, thyroxine or free thyroxine was found among their breastfed infants at day 5 to 7 postpartum. Studies in Africa have used chlorhexidine vaginally prior to delivery in an attempt to reduce the frequency of mother-to-child transmission (MTCT) of HIV. In one, cotton soaked in 0.25% chlorhexidine solution was used to swab the vaginal walls every 4 hours from admission into labor until delivery in 4078 women. The other study used 120 mL of either 0.2% or 0.4% chlorhexidine solution as a vaginal lavage every 3 hours from admission to labor until delivery in 309 women. The average number of lavages was 2.1 (range 1 to 11). Chlorhexidine 0.25% swabs reduced MTCT in patients whose membranes ruptured more than 4 hours before delivery, but not in other women. Vaginal lavage showed a statistically nonsignificant trend towards reduction of MTCT, with the 0.4% greater than the 0.2%. Almost all of the infants in these studies were breastfed. No adverse events were reported in the infants, but follow-up related primarily to infant mortality and HIV status rather than effects of chlorhexidine. ◉ Effects on Lactation and Breastmilk A randomized study compared 0.2% chlorhexidine in alcohol to distilled water as a spray to the breast in 200 mothers who were nursing newborns. The mothers sprayed their breasts with the liquid before and after each feeding. Mothers and infants were assessed at discharge and weekly thereafter. Discomfort and nipple trauma were less frequent in the chlorhexidine group than in the placebo group, particularly at the first assessment. Although skin flora on the breasts of the treated mothers was reduced, there was no difference in the frequency of mastitis between the treated and placebo groups. No obvious side effects occurred in the breastfed infants and there were no differences in the rates of oral thrush in infants between the treatments. A systematic review concluded that this practice is not justified based on current evidence. Protein Binding Chlorhexidine is known to bind albumin in both serum and saliva, though the extent of this binding is unclear. |
| 参考文献 |
|
| 其他信息 |
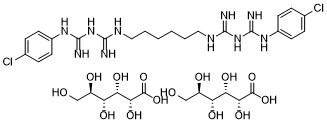
Chlorhexidine gluconate is an organochlorine compound and a D-gluconate adduct. It has a role as an antibacterial agent. It is functionally related to a chlorhexidine.
Chlorhexidine is a broad-spectrum antimicrobial biguanide used as a topical antiseptic and in dental practice for the treatment of inflammatory dental conditions caused by microorganisms. It is one of the most common skin and mucous membrane antiseptic agents in use today. The molecule itself is a cationic bis-guanide consisting of two 4-chlorophenyl rings and two biguanide groups joined by a central hexamethylene chain. Topical chlorhexidine for disinfection, as well as oral rinses for dental use, carries activity against a broad range of pathogens including bacteria, yeasts, and viruses. Chlorhexidine was developed in the UK by Imperial Chemical Industries in the early 1950s and was introduced to the US in the 1970s. The FDA withdrew its approval for the use of chlorhexidine gluconate topical tincture 0.5%, due to a significant number of reports concerning chemical and thermal burns associated with the use of this product. Other formulations of chlorhexidine continue to be available. Chlorhexidine is a biguanide compound used as an antiseptic agent with topical antibacterial activity. Chlorhexidine is positively charged and reacts with the negatively charged microbial cell surface, thereby destroying the integrity of the cell membrane. Subsequently, chlorhexidine penetrates into the cell and causes leakage of intracellular components leading to cell death. Since gram positive bacteria are more negatively charged, they are more sensitive to this agent. Chlorhexidine Gluconate is the gluconate salt form of chlorhexidine, a biguanide compound used as an antiseptic agent with topical antibacterial activity. Chlorhexidine gluconate is positively charged and reacts with the negatively charged microbial cell surface, thereby destroying the integrity of the cell membrane. Subsequently, chlorhexidine gluconate penetrates into the cell and causes leakage of intracellular components leading to cell death. Since gram positive bacteria are more negatively charged, they are more sensitive to this agent. See also: Chlorhexidine Gluconate; Isopropyl Alcohol (component of); Alcohol; Chlorhexidine Gluconate (component of); Benzethonium chloride; chlorhexidine gluconate (component of) ... View More ... Drug Indication Chlorhexidine is available over-the-counter in various formulations (e.g. solution, sponge, cloth, swab) as a topical antiseptic to sanitize prior to surgeries and/or medical procedures. Dental formulations, available by prescription only, include an oral rinse indicated for the treatment of gingivitis and a slow-release "chip" which is inserted into periodontal pockets and is indicated for the reduction of pocket depth in adult patients with periodontitis as an adjunct therapy to dental scaling and root planing procedures. FDA Label Mechanism of Action Chlorhexidine’s broad-spectrum antimicrobial effects are due to its ability to disrupt microbial cell membranes. The positively charged chlorhexidine molecule reacts with negatively charged phosphate groups on microbial cell surfaces - this reaction both destroys the integrity of the cell, allowing leakage of intracellular material, and allows chlorhexidine to enter the cell, causing precipitation of cytoplasmic components and ultimately cell death. The specific means of cell death is dependent on the concentration of chlorhexidine - lower concentrations are bacteriostatic and result in leakage of intracellular substances such as potassium and phosphorous, whereas higher concentrations are bactericidal and cause cytoplasmic precipitation. |
| 分子式 |
C28H40CL2N10O7
|
|---|---|
| 分子量 |
699.59
|
| 精确质量 |
896.319
|
| CAS号 |
18472-51-0
|
| 相关CAS号 |
Chlorhexidine dihydrochloride;3697-42-5;Chlorhexidine;55-56-1;Chlorhexidine diacetate;56-95-1;Chlorhexidine acetate hydrate;206986-79-0
|
| PubChem CID |
9552081
|
| 外观&性状 |
Colorless to light yellow liquid
|
| 密度 |
1.06 g/mL at 25 °C(lit.)
|
| 沸点 |
699.3ºC at 760 mmHg
|
| 熔点 |
134ºC
|
| 闪点 |
376.7ºC
|
| 蒸汽压 |
0mmHg at 25°C
|
| tPSA |
444.48
|
| 氢键供体(HBD)数目 |
18
|
| 氢键受体(HBA)数目 |
16
|
| 可旋转键数目(RBC) |
23
|
| 重原子数目 |
60
|
| 分子复杂度/Complexity |
819
|
| 定义原子立体中心数目 |
8
|
| SMILES |
N=C(NC(NCCCCCCNC(NC(NC1=CC=C(Cl)C=C1)=N)=N)=N)NC2=CC=C(Cl)C=C2.O[C@H]([C@@H](O)C(O)=O)[C@H](O)[C@H](O)CO.O[C@H]([C@@H](O)C(O)=O)[C@H](O)[C@H](O)CO
|
| InChi Key |
YZIYKJHYYHPJIB-UUPCJSQJSA-N
|
| InChi Code |
InChI=1S/C22H30Cl2N10.2C6H12O7/c23-15-5-9-17(10-6-15)31-21(27)33-19(25)29-13-3-1-2-4-14-30-20(26)34-22(28)32-18-11-7-16(24)8-12-18;2*7-1-2(8)3(9)4(10)5(11)6(12)13/h5-12H,1-4,13-14H2,(H5,25,27,29,31,33)(H5,26,28,30,32,34);2*2-5,7-11H,1H2,(H,12,13)/t;2*2-,3-,4+,5-/m.11/s1
|
| 化学名 |
(1E)-2-[6-[[amino-[(E)-[amino-(4-chloroanilino)methylidene]amino]methylidene]amino]hexyl]-1-[amino-(4-chloroanilino)methylidene]guanidine;(2R,3S,4R,5R)-2,3,4,5,6-pentahydroxyhexanoic acid
|
| 别名 |
Chlorhexidine digluconate UniseptChlorhexidine Gluconate Peridex GibitanUNII-MOR84MUD8E Hexidine Hibiclens Hibident Hibisol HibitaneHibiscrub Perio Chip
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
H2O : ~100 mg/mL (~111.39 mM)
DMSO : ≥ 38 mg/mL (~42.33 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 100 mg/mL (111.39 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。
请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.4294 mL | 7.1470 mL | 14.2941 mL | |
| 5 mM | 0.2859 mL | 1.4294 mL | 2.8588 mL | |
| 10 mM | 0.1429 mL | 0.7147 mL | 1.4294 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。