| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Caffeine is rapidly absorbed after oral or parenteral administration, reaching peak plasma concentration within 30 minutes to 2 hours after administration. After oral administration, onset of action takes place within 45 to 1 hour. Food may delay caffeine absorption. The peak plasma level for caffeine ranges from 6-10mg/L. The absolute bioavailability is unavailable in neonates, but reaches about 100% in adults. The major metabolites of caffeine can be found excreted in the urine. About 0.5% to 2% of a caffeine dose is found excreted in urine, as it because it is heavily absorbed in the renal tubules. Caffeine has the ability to rapidly cross the blood-brain barrier. It is water and fat soluble and distributes throughout the body. Caffeine concentrations in the cerebrospinal fluid of preterm newborns are similar to the concentrations found in the plasma. The mean volume of distribution of caffeine in infants is 0.8-0.9 L/kg and 0.6 L/kg in the adult population. The clearance of caffeine varies, but on average, is about 0.078 L/kg/h (1.3 mL/min/kg). World-wide, many fetuses and infants are exposed to methylxanthines via maternal consumption of coffee and other beverages containing these substances. Methylxanthines (caffeine, theophylline and aminophylline) are also commonly used as a medication for apnea of prematurity. ... Methylxanthines readily passes the placenta barrier and enters all tissues and thus may affect the fetus/newborn at any time during pregnancy or postnatal life, given that the effector systems are mature. ... Caffeine and citrated caffeine are well absorbed following oral administration. Absorption of caffeine following oral administration may be more rapid than that following IM injection of caffeine and sodium benzoate. Absorption following rectal administration of caffeine in suppositories may be slow and erratic. ... Following oral administration of 100 mg of caffeine (as coffee), peak plasma concentrations of about 1.5-1.8 ug/mL are reached after 50-75 minutes. After oral administration of 10 mg caffeine base/kg to preterm neonates, the peak plasma concentration for caffeine ranged from 6-10 mg/L and the mean time to reach peak concentration /Tmax/ ranged from 30 minutes to 2 hours. The /Tmax/ was not affected by formula feeding. Caffeine is rapidly distributed into body tissues, readily crossing the placenta and blood-brain barrier. Caffeine concentration in the CSF fluid of preterm neonates approximates the plasma concentration. The mean volume of distribution of caffeine in infants (0.8-0.9 L/kg) is slightly higher than that in adults (0.6 L/kg). ... Caffeine has been shown to distribute into milk in a milk-to-serum concentration ratio of 0.5-0.76. For more Absorption, Distribution and Excretion (Complete) data for CAFFEINE (11 total), please visit the HSDB record page. Metabolism / Metabolites Caffeine metabolism occurs mainly in the liver via the cytochrome CYP1A2 enzyme. The products of caffeine metabolism include paraxanthine, theobromine, and theophylline. The first step of caffeine metabolism is demethylation, yielding paraxanthine (a major metabolite), followed by theobromine, and theophylline, which are both minor metabolites. They are then excreted in urine as urates after additional metabolism. The enzymes xanthine oxidase and N-acetyltransferase 2 (NAT2) also participate in the metabolism of caffeine. Caffeine is metabolized by the cytochrome P-450 (CYP) enzyme system, principally by isoenzyme 1A2. Therefore, caffeine has the potential to interact with drugs that are metabolized by CYP1A2 or with drugs that induce or inhibit this isoenzyme. In adults, the drug is rapidly metabolized in the liver to 1-methyluric acid, 1-methylxanthine, and 7-methylxanthine. Interconversion between caffeine and theophylline has been reported in preterm neonates... In-vivo and in-vitro experiments showed a progressive increase in the activity of the hepatic microsomal enzymes that metabolize caffeine during neonatal development. In beagle puppies, change in caffeine clearance was determined by the rate of maturation of caffeine-7-demethylase. Caffeine is eliminated in animals by biotransformation in the liver to dimethylxanthines, dimethyl- and monomethyluric acids and uracil derivatives; important quantitative differences have been demonstrated in the formation and elimination of metabolites in rats, mice and Chinese hamsters. These differences are even more important in monkeys, where caffeine is almost completely metabolized to theophylline. ... Some species-dependent metabolites have been identified. Trimethylallantoin was first reported in rats. A ... derivative of paraxanthine was found in mice and identified as the 3-beta-D-glucuronide of paraxanthine. Methylated ureas and sulfur-containing derivatives found in urine in trace amounts are produced by the intestinal flora. In contrast, the acetylated uracil derivative, 5-acetylamino-6-formylamino-3-methyluracil, one of the most important caffeine metabolites in humans, has not been identified in rodents or other animal species. Other uracil derivatives produced from caffeine, theobromine and paraxanthine in rats were found in human urine. In rats, the hepatic demethylation of caffeine shows an age-related decline, resulting in a greatly increased elimination half-time in older adult rats. Caffeine metabolism is qualitatively relatively similar in animals and humans ... . The main metabolic pathways are: demethylation and hydroxylation of the 8-position leading to the formation of the respective uracil and uric acid derivatives. There are, however, some quantitative differences in the metabolic profile. Humans are characterized by the importance of 3-methyl demethylation leading to the formation of paraxanthine and especially metabolites thereof through subsequent metabolic steps. The main urinary metabolites in humans are 1-methyluric acid, 1-methylxanthine, 5-acetylamino-6-formylamino-3- methyluracil (not found in rats and mice), 1,7-dimethyluric acid and paraxanthin. In rats and mice, the metabolism of caffeine is predominantly via theobromine and theophylline. The main urinary metabolites are 1,3-dimethyluracil, paraxanthine, trimethyluric acid, theophylline, and theobromine. Caffeine metabolism decreases during pregnancy, resulting in higher serum concentrations. Caffeine has known human metabolites that include Theobromine, theophylline, 1,3,7-Trimethyluric acid, and paraxanthine. Hepatic cytochrome P450 1A2 (CYP 1A2) is involved in caffeine biotransformation. About 80% of a dose of caffeine is metabolized to paraxanthine (1,7-dimethylxanthine), 10% to theobromine (3,7-dimethylxanthine), and 4% to theophylline (1,3-dimethylxanthine). Route of Elimination: In young infants, the elimination of caffeine is much slower than that in adults due to immature hepatic and/or renal function. Half Life: 3 to 7 hours in adults, 65 to 130 hours in neonates Biological Half-Life In an average-sized adult or child above the age of 9, the half-life of caffeine is approximately 5 hours. Various characteristics and conditions can alter caffeine half-life. It can be reduced by up to 50% in smokers. Pregnant women show an increased half-life of 15 hours or higher, especially in the third trimester. The half-life in newborns is prolonged to about 8 hours at full-term and 100 hours in premature infants, likely due to reduced ability to metabolize it. Liver disease or drugs that inhibit CYP1A2 can increase caffeine half-life. Elimination 1/2 life in adults = 2.5-4.5 hours; [Reference #1] Caffeine has a plasma half-life (t1/2) of 3 to 5 hours in adults. In one study, when administered to pregnant women prior to delivery, caffeine had a prolonged mean half-life of 80 hours in neonates after delivery. Mean half-life /T 1/2/ and fraction excreted unchanged in urine of caffeine in infants have been shown to be inversely related to gestational/postconceptual age. In neonates, the /T 1/2/ is approximately 3-4 days... The half-time for caffeine is 0.7-1.0 hr in rats and mice, 1-1.6 hr in rabbits, 3-5 hr in monkeys, 4-4.3 hr in dogs and 11-12 hr in baboons. /The authors/ studied 17 preterm infants receiving caffeine, and measured their plasma levels of caffeine and the theophylline metabolite by high-pressure liquid chromatography. The half-life was calculated by computer analysis using the least-square method. The mean gestational age of our patients was 29.7 +/- 1.9 weeks (mean +/- SD) and they were studied at 20.7 +/- 6.6 days (mean +/- SD) postnatal age. The caffeine half-life was 52.03 +/- 23.87 hr (means +/- SD) and the theophylline half-life was 77.04 +/- 65.01 hr (mean +/- SD). |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Caffeine stimulates medullary, vagal, vasomotor, and respiratory centers, promoting bradycardia, vasoconstriction, and increased respiratory rate. This action was previously believed to be due primarily to increased intracellular cyclic 3′,5′-adenosine monophosphate (cyclic AMP) following inhibition of phosphodiesterase, the enzyme that degrades cyclic AMP. It is now thought that xanthines such as caffeine act as antagonists at adenosine-receptors within the plasma membrane of virtually every cell. As adenosine acts as an autocoid, inhibiting the release of neurotransmitters from presynaptic sites but augmenting the actions of norepinephrine or angiotensin, antagonism of adenosine receptors promotes neurotransmitter release. This explains the stimulatory effects of caffeine. Blockade of the adenosine A1 receptor in the heart leads to the accelerated, pronounced "pounding" of the heart upon caffeine intake. Toxicity Data LD50: 127 mg/kg (Oral, Mouse) (A308) Interactions When caffeine and disulfiram are administered concomitantly...the total blood clearance of caffeine is substantially decreased and its elimination half-life is increased. ... Cocaine and caffeine's independent effects on cardiodynamics are documented but to our knowledge combined effects of both on complete cardiovascular hemodynamics remains to be examined. Eighteen dogs were instrumented to pass cardiac catheters into right and left heart. The experiments were performed after they recovered from the effects of anesthesia. In phase I (30 experiments on 8 dogs), the doses were established by dose-response curve. In phases II and III, another 10 dogs were subjected to 28 experiments. They were given i.v. cocaine followed by caffeine and vice versa to study their effects on hemodynamics and coronary flow reserve. Phase 1: The doses of cocaine (2 mg/kg) and caffeine (5 mg/kg) were established. Phase II: Cocaine increased heart rate, blood pressure and dP/dt but coronary flow reserve (CFR) decreased significantly. Caffeine administered after cocaine attenuated these effects (dP/dt decreased to 4910 + or -104 from 5066 + or - 110 mm Hg s; p The effects of the widely consumed drugs caffeine and phenylpropanolamine are mediated through activation of the central and sympathetic nervous systems. Severe, life-threatening, and occasionally fatal hypertensive reactions have been reported after their combined use. This study examined the possible pharmacokinetic interaction of phenylpropanolamine and caffeine. Sixteen normal subjects received combinations of caffeine, phenylpropanolamine, and placebo. In subjects receiving 400 mg caffeine plus 75 mg phenylpropanolamine, the mean (+/- SEM) peak plasma caffeine concentration of 8.0 +/- 2.2 micrograms/mL was significantly greater than after 400 mg caffeine alone (2.1 +/- 0.3 micrograms/mL; t[24] = 2.4; p less than 0.01). Physical side effects were more frequent after the phenylpropanolamine-caffeine combination than after either drug alone or after placebo. Greater increases in both systolic and diastolic blood pressures occurred after the combination than after either drug alone. Because caffeine levels can be increased greatly when certain other drugs are coconsumed, these data indicate that phenylpropanolamine may enhance absorption or inhibit elimination of caffeine and may explain increased side effects reported after their combined use. For more Interactions (Complete) data for CAFFEINE (21 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Rat ip 260 mg/kg LD50 Rat oral 192 mg/kg LD50 Rat rectal 300 mg/kg LD50 Rat iv 105 mg/kg For more Non-Human Toxicity Values (Complete) data for CAFFEINE (13 total), please visit the HSDB record page. |
| 其他信息 |
Therapeutic Uses
Central Nervous System Stimulants; Phosphodiesterase Inhibitors; Purinergic P1 Receptor Antagonists Caffeine is used orally as a mild CNS stimulant to aid in staying awake and to restore mental alertness in fatigued patients. Apnea of prematurity. Caffeine citrate is used iv or orally in the short-term (10-12 days) treatment of apnea of prematurity in neonates who are between 28 and less than 33 weeks of gestational age. Caffeine is designated an orphan drug by the US Food and Drug Administration (FDA) for use in apnea in premature neonates. Caffeine is used in combination with ergotamine tartrate to abort vascular headaches such as migraine and cluster headaches (histamine cephalalgia). For more Therapeutic Uses (Complete) data for CAFFEINE (11 total), please visit the HSDB record page. Drug Warnings Because it has been suggested that caffeine may promote gastric ulceration, the drug should be used cautiously in patients with a history of peptic ulcer. Because of its suspected arrhythmogenic potential, it is generally recommended that caffeine be avoided in patients with symptomatic cardiac arrhythmias and/or palpitations and during the first several days to weeks after an acute myocardial infarction Prior to initiation of caffeine citrate therapy, baseline serum concentrations of caffeine should be measured in neonates previously treated with theophylline, since preterm neonates metabolize theophylline to caffeine. Similarly, baseline serum concentrations of caffeine should be measured in infants born to mothers who consumed caffeine prior to delivery since caffeine readily crosses the placenta. Serious toxicity has been reported when serum caffeine concentrations exceed 50 ug/mL. /Caffeine citrate/ In clinical trials reported in the literature, cases of hypoglycemia and hyperglycemia have been reported in patients receiving caffeine; therefore, blood glucose concentration may need to be monitored periodically in neonates receiving caffeine citrate. /Caffeine citrate/ During the placebo-controlled trial of caffeine citrate establishing efficacy in the US for apnea of prematurity, 6 cases of necrotizing enterocolitis developed among the 85 neonates studied, 3 cases of which were fatal. Five of the 6 neonates had been randomized to treatment with or had been exposed to caffeine citrate. Reports in the literature have raised the possibility of an association betwen the use of methylxanthines and the development of necrotizing enterocolitis, although a causal relationship between methylxanthine use and the development of necrotizing enterocolitis have not been established. Therefore, as with all premature neonates, patients being treated with caffeine citrate should be monitored carefully for the development of necrotizing enterocolitis. /Caffeine citrate/ For more Drug Warnings (Complete) data for CAFFEINE (25 total), please visit the HSDB record page. Pharmacodynamics Caffeine stimulates the central nervous system (CNS), heightening alertness, and sometimes causing restlessness and agitation. It relaxes smooth muscle, stimulates the contraction of cardiac muscle, and enhances athletic performance. Caffeine promotes gastric acid secretion and increases gastrointestinal motility. It is often combined in products with analgesics and ergot alkaloids, relieving the symptoms of migraine and other types of headaches. Finally, caffeine acts as a mild diuretic. |
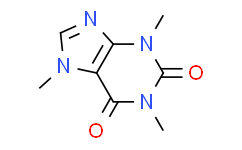
| 分子式 |
C8H10N4O2
|
|---|---|
| 分子量 |
194.19060087204
|
| 精确质量 |
194.08
|
| CAS号 |
58-08-2
|
| PubChem CID |
2519
|
| 外观&性状 |
White, prismatic crystals
Hexagonal prisms White, fleecy masses or long, flexible, silky crystals |
| 熔点 |
460 °F (NTP, 1992)
235-237 236.2 °C 238 °C 235 °C |
| LogP |
-0.1
|
| tPSA |
58.4
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
3
|
| 可旋转键数目(RBC) |
0
|
| 重原子数目 |
14
|
| 分子复杂度/Complexity |
293
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
RYYVLZVUVIJVGH-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C8H10N4O2/c1-10-4-9-6-5(10)7(13)12(3)8(14)11(6)2/h4H,1-3H3
|
| 化学名 |
1,3,7-trimethylpurine-2,6-dione
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 5.1496 mL | 25.7480 mL | 51.4960 mL | |
| 5 mM | 1.0299 mL | 5.1496 mL | 10.2992 mL | |
| 10 mM | 0.5150 mL | 2.5748 mL | 5.1496 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Study to Investigate the Effect of Rocatinlimab (AMG 451) on the Pharmacokinetics of Multiple Cytochrome P450 (CYP450) Substrates in Participants With Moderate to Severe Atopic Dermatitis
CTID: NCT05891119
PhaseEarly Phase 1 Status: Active, not recruiting
Date: 2024-11-07